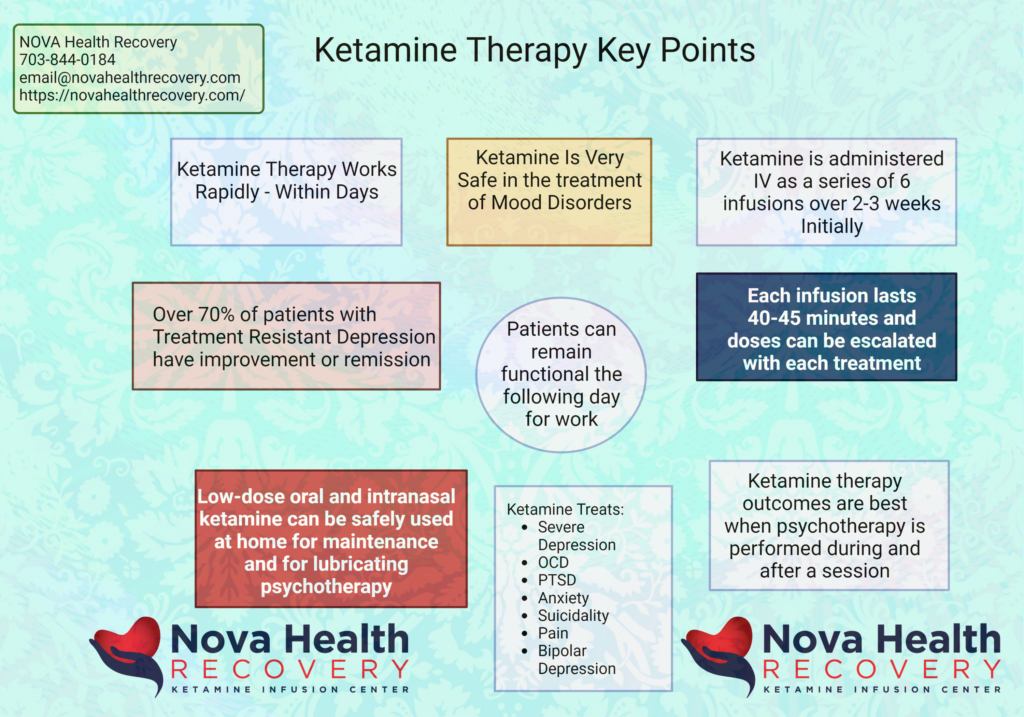
Ketamine therapy and psychedelics represent state-of-the-art treatments for mood disorders that target neural circuitry and neurotransmitter systems that are not treated by traditional medications. There are currently clinical trials of MDMA and psilocybin that are ongoing and quite positive. However, only ketamine is available for current use in the treatment of depression in several other mood disorders. Ketamine is rapid acting and robust in the treatment of depression. Over 70% of patients who have failed multiple other therapies have improvement or remission with Ketamine therapy. Ketamine is safe, effective, and has a low risk of abuse. Psychotherapy, along with psychedelic treatments, not only augments the process but makes the treatment last longer.
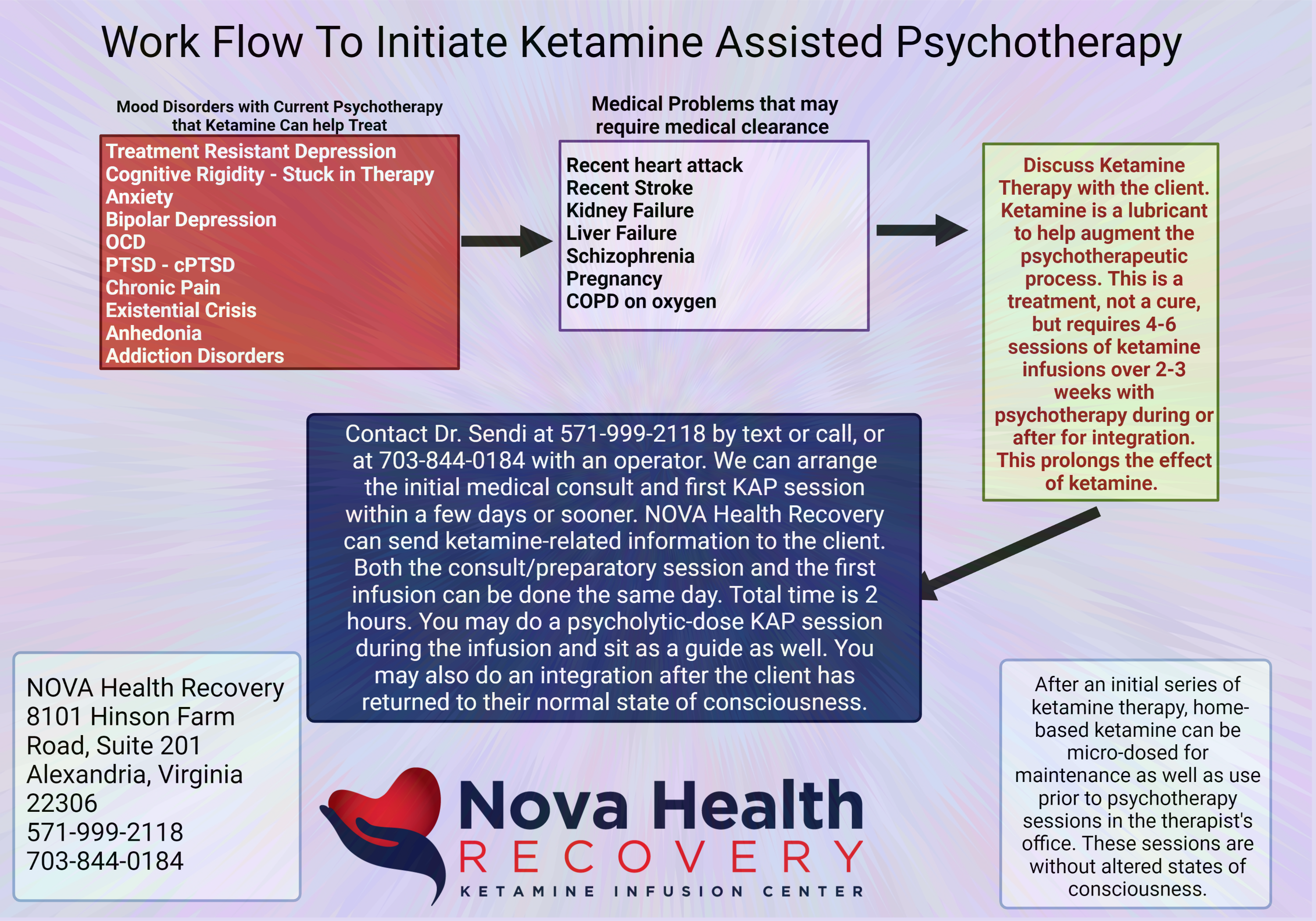
If you are a therapist currently working with patients, ketamine therapy can be immediately introduced into your practice to help augment your workflow with patients and increase successful results. Ketamine therapy can improve depression and other mood disorders rapidly, and cognitive behavioral therapy with other tools of psychotherapy can augment the ketamine treatment as well in the form of ketamine-assisted psychotherapy. Nova health recovery ketamine infusion center offers therapists the opportunity to guide their patients in the office during the ketamine sessions. Likewise, the patients can benefit from integration sessions later that day or the following day. Even if you have no experience directly with ketamine treatments, Nova Health Recovery can assist you in the treatment process and help you monitor your clients at no cost to you.
Who benefits from ketamine treatments?
⦁ Treatment-resistant depression
⦁ New onset depression
⦁ Generalized anxiety disorders
⦁ PTSD
⦁ Obsessive-compulsive disorder
⦁ Bipolar depression
⦁ Existential crisis
⦁ Chronic pain
⦁ Addiction disorders such as alcoholism, cocaine use disorder, and opiate use disorder.
⦁ Patients who are stuck in therapy and are suffering from hamster wheel ruminations and negativity.
Generally, patients will get 2 to 3 infusions per week, each lasting one hour. The patients can receive guided therapy by the therapist during the infusion in the room, or after the infusion in the same room, as well as later in the day or the next day for integration of new concepts that were learned during the experiential. This allows the patient to consolidate new learning for the purposes of psychological flexibility, improved coping skills, and better mood. The purpose of this webpage is to inform therapists of these options and the process by which ketamine treatments work. We welcome you to reach out to Dr.Sendi and NOVA Health Recovery Ketamine Infusion Center for questions concerning this process, more information, or how you can arrange times for your clients and you to start ketamine-assisted psychotherapy (KAP). The number to call direct is 571-999-2118 (Christopher Sendi, M.D.)
If you are a therapist looking to incorporate Ketamine and ketamine-assisted psychotherapy (KAP) into your practice, email NOVA Health Recovery below or at email@novahealthrecovery.com. Also, you may contact Dr. Sendi by cell/text at 571-999-2118. There is no cost to the therapist to perform KAP therapy on their clients at NOVA Health Recovery:
If You are a Therapist Looking to Immediately Incorporate Ketamine-Assisted Psychotherapy Into Your Practice:
Click the Link Below to Contact NOVA Health Recovery Regarding KAP Therapy for your Practice:
What Is Ketamine?
What is Ketamine?
The fancy name for ketamine is:
2-(2-chlorophenyl)-2-(methylamino)-cyclohexan-1-one
It is an arylcycloalkamine and is structurally related to cyclidines, such as phencyclidine (PCP). It is synthesized using the reagents o-chlorobenzonitrile and cyclopentyl grignard. Ketamine is a racemic mixture of S-(+)-ketamine and R-(-)-ketamine, and it acts as a NMDA receptor antagonist. Ketamine modulates the glutamate system, which is different from traditional antidepressant therapies.
Ketamine has been used for both anesthetic purposes and for veterinarian surgical procedures as well.
Ketamine is available as a hydrochloride salt or freebase, and it is water-soluble. It’s availability in the body depends on the route with which it is administered. See the table below:
Route Bioavailability
| Intramuscular | 93% |
| Intranasal | 50% |
| Intravenous | 100% |
| Oral | 20% |
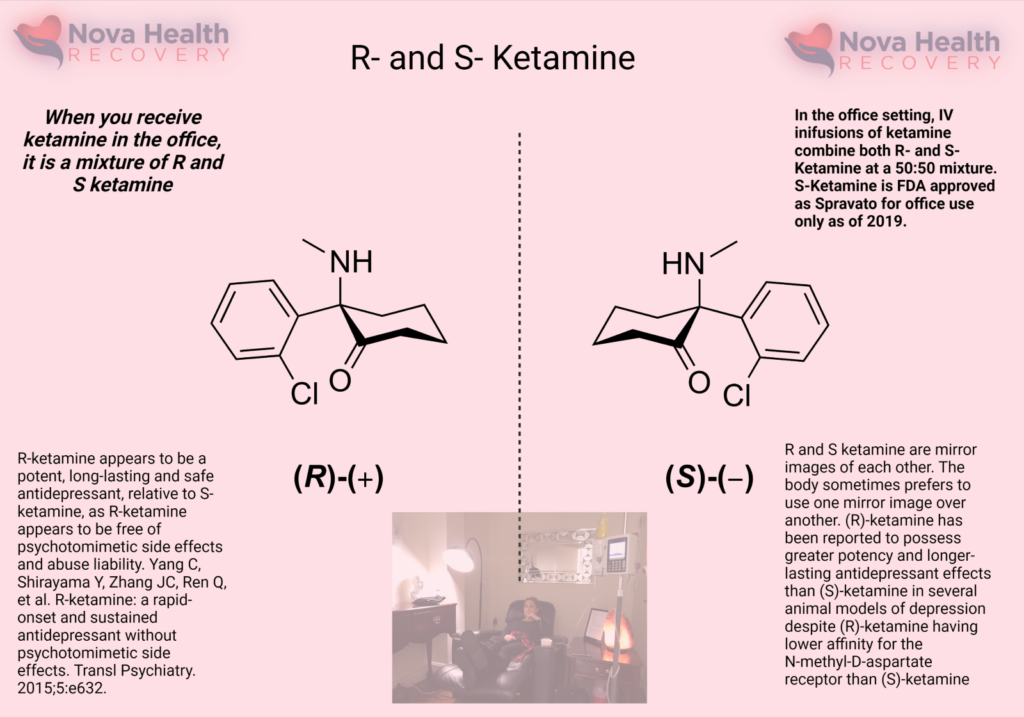
The left-handed form of ketamine or S-ketamine is otherwise known as Spravato, which is an FDA-approved nasal spray of ketamine that has been available since 2019. It is taken alongside an oral antidepressant medication for treatment-resistant depression. Intravenous ketamine is given as a racemic mixture, in which both the right- and left-handed forms of ketamine are administered. The different enantiomers of ketamine, which refers to either the right- or left-handed ketamine, have different pharmacological activity, tissue uptake, metabolism, and receptor affinity.
Pharmacokinetics: Ketamine is highly liposoluble with low protein binding ability, which enables rapid transfer across the blood-brain barrier. Concentrations of ketamine in the brain are often 4-5 times higher than that in the blood plasma. It takes between 7 – 11 minutes for the plasma concentration of ketamine to reduce by 50%.
Ketamine enantiomers:
S-ketamine has a higher affinity for the NMDA receptor and so lower doses are required to achieve effect. (1)(2) As lower doses of S-ketamine are required to elicit effects, there is probably less drowsiness, agitation, and cognitive issues when it is administered. S-ketamine has a 2-3 fold higher affinity for the opioid receptor than R-ketamine.
R-ketamine has a lower NMDA receptor affinity and is not used alone currently. There are studies demonstrating that this enantiomer induces longer antidepressant effects and higher rates of synaptogenesis relative to the S version. (3)(4)(5) The R version also has less dissociation and sensory deficits as well when it is administered. (6)
Ketamine Metabolism:
Ketamine is primarily metabolized via oxidative N-demethylation of the cyclohexanone ring by the CYP450 enzyme, producing the primary and active metabolite, norketamine (80%) which is hydroxylated to hydroxy-norketamine (15%) and conjugated with glucoronate and excreted in the urine.
How does ketamine interact with receptors in the brain?
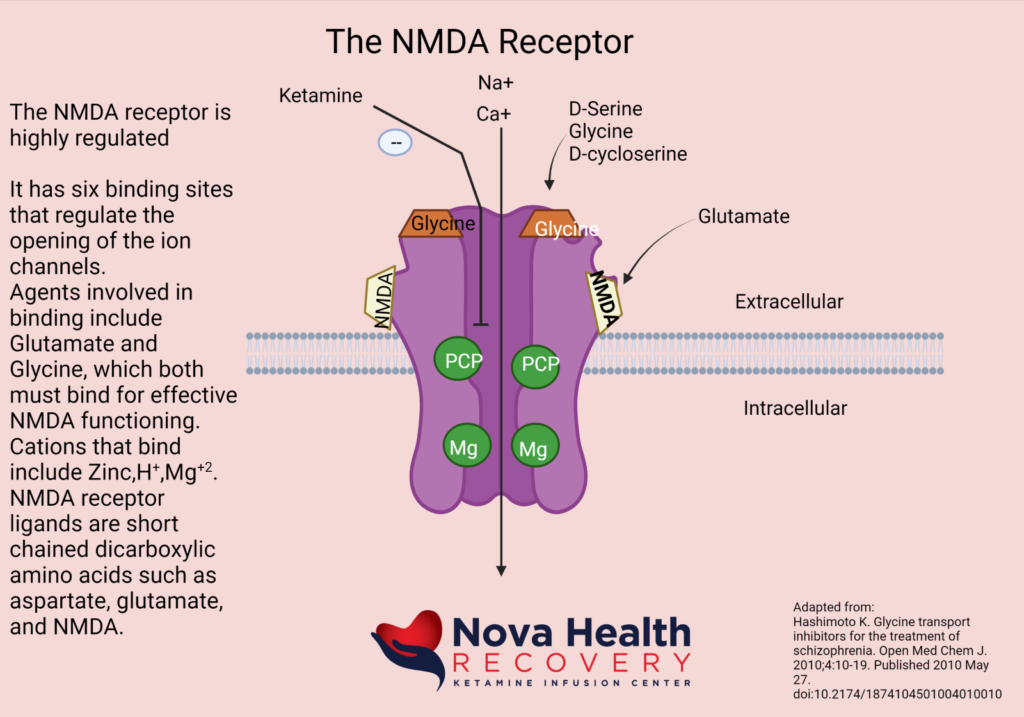
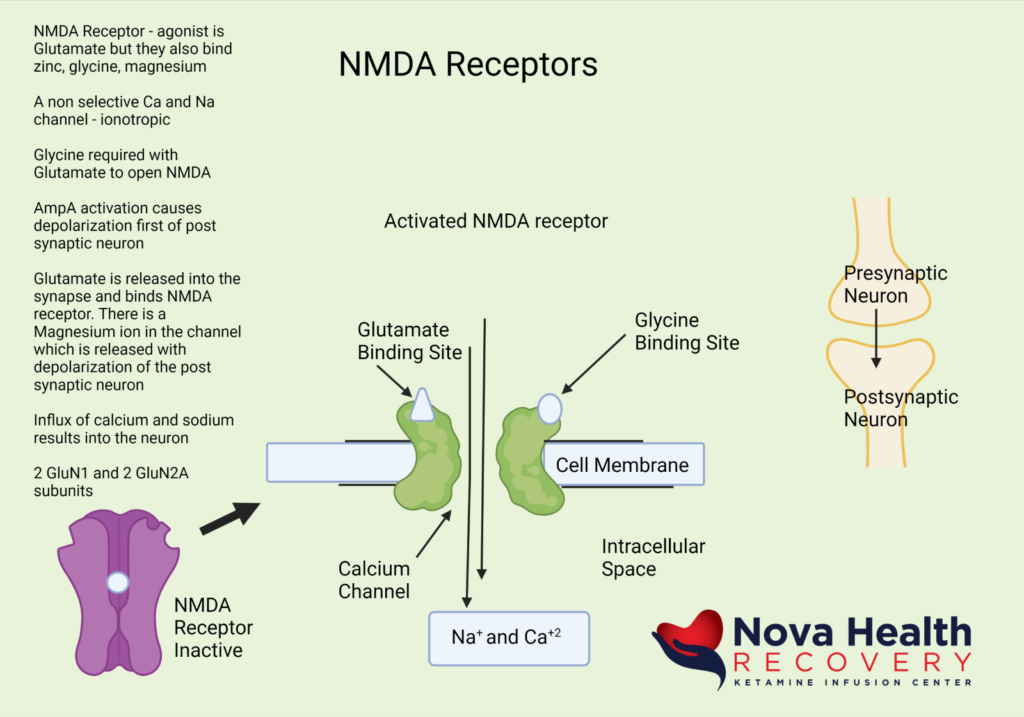
Ketamine binds the numerous receptors, but its main effect is through its activity as a non-competitive NMDA receptor antagonist, where it blocks the PCP binding site of the NMDA receptor and prevents depolarization of the neuron. Generally speaking, the NMDA receptor is an excitatory receptor playing a role in learning and sensory perception. Ketamine also interacts with other receptors at higher doses, such as the opioid receptors, which may contribute to the anti-pain (antinociceptive) effects of ketamine. (7)(8) Ketamine also interacts with the HCN1 and sigma receptors as an antagonist. It is also an antagonist at muscarinic CNS receptors and agonistic (activating) at alpha- and beta-adrenergic receptors.
What does the NMDA Receptor look like? How is the NMDA receptor Activated?
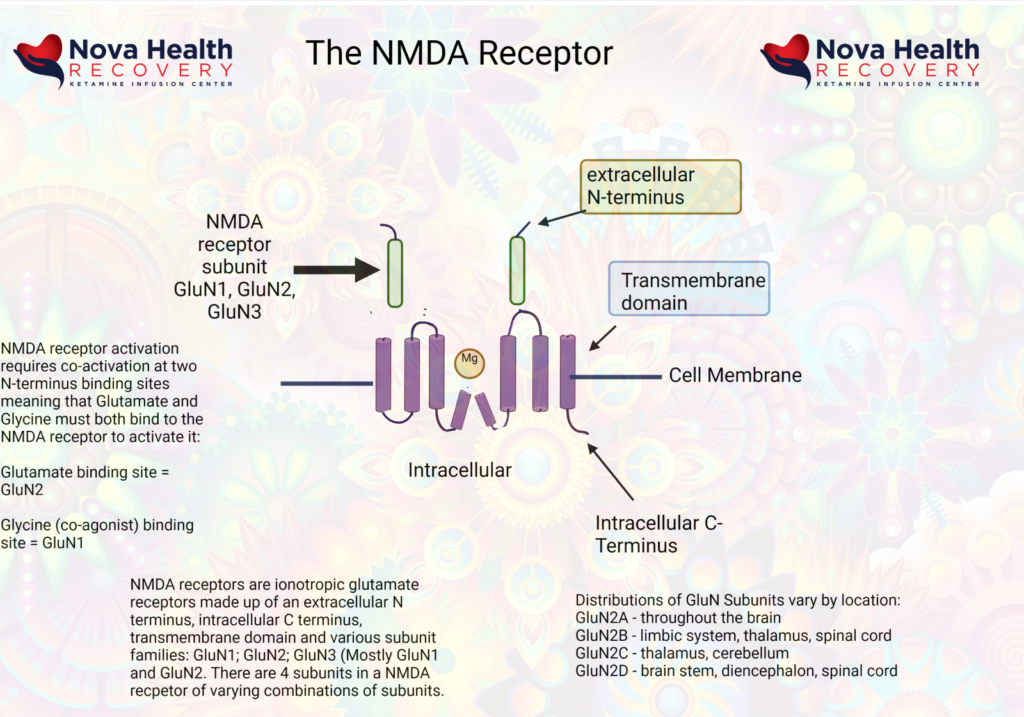
Magnesium blocks the NMDA receptor and prevents inflow of Na+ and Ca+2:
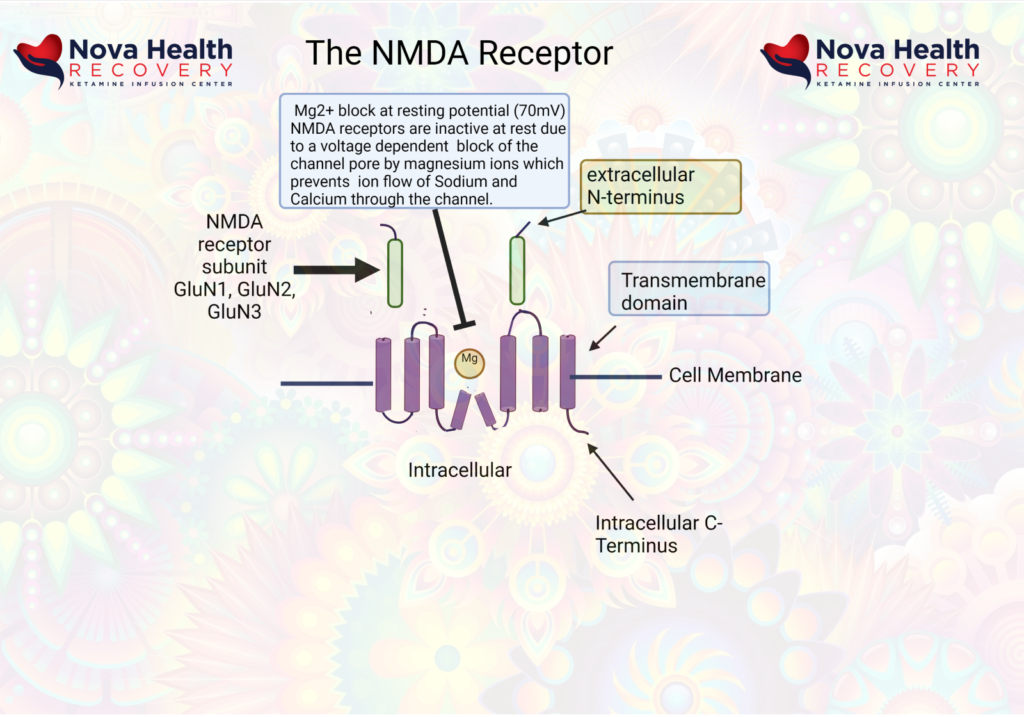
The post-synaptic neuron needs to be depolarized enough to allow the Magnesium ion to be displaced. This first occurs through activation of the AMPA receptor, which also is a receptor that binds/responds to glutamate and is present where there are NMDA receptors.
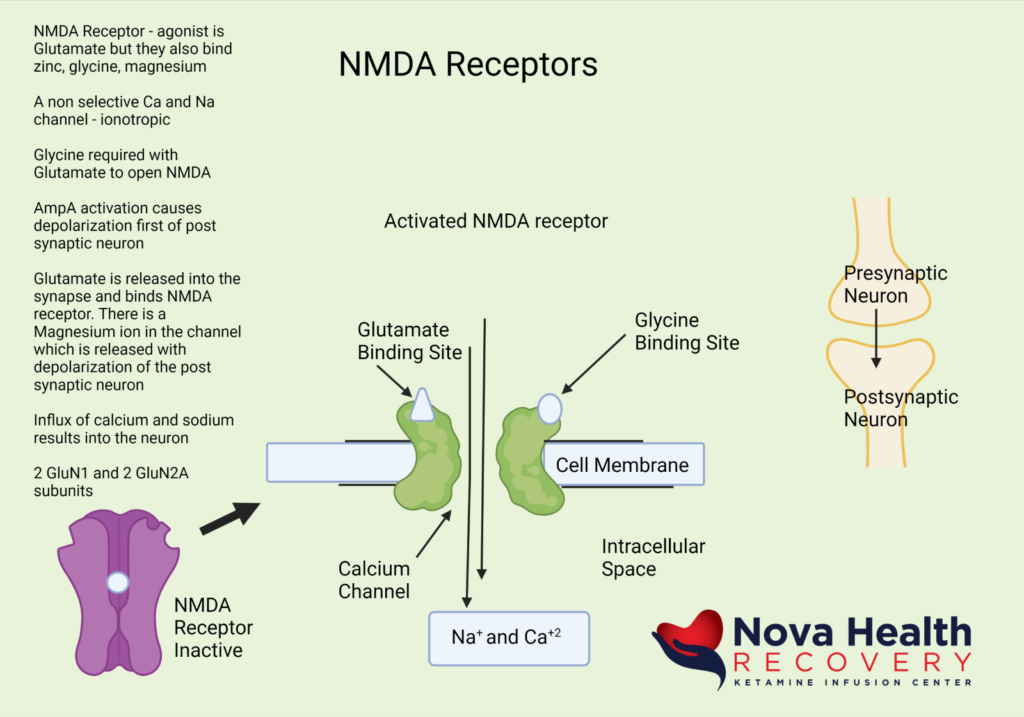
So, the AMPA receptor gets activated first with glutamate binding and allows a current of sodium ions into the post synaptic neuron, which then depolarizes the neuron and pushes out the Magnesium ion in the NMDA channel. The NMDA receptor now can allow sodium and calcium ions into the post-synaptic neuron to cause downstream protein production (BDNF and synaptogenesis).
Again, the sequence of NMDA receptor activation is:
- Low-level background glutamate release by pre-synaptic neuron interacts with NMDA and AMPA receptors. The AMPA receptors are more reactive initially and allow sodium into the post-synaptic neuron, which depolarizes it.
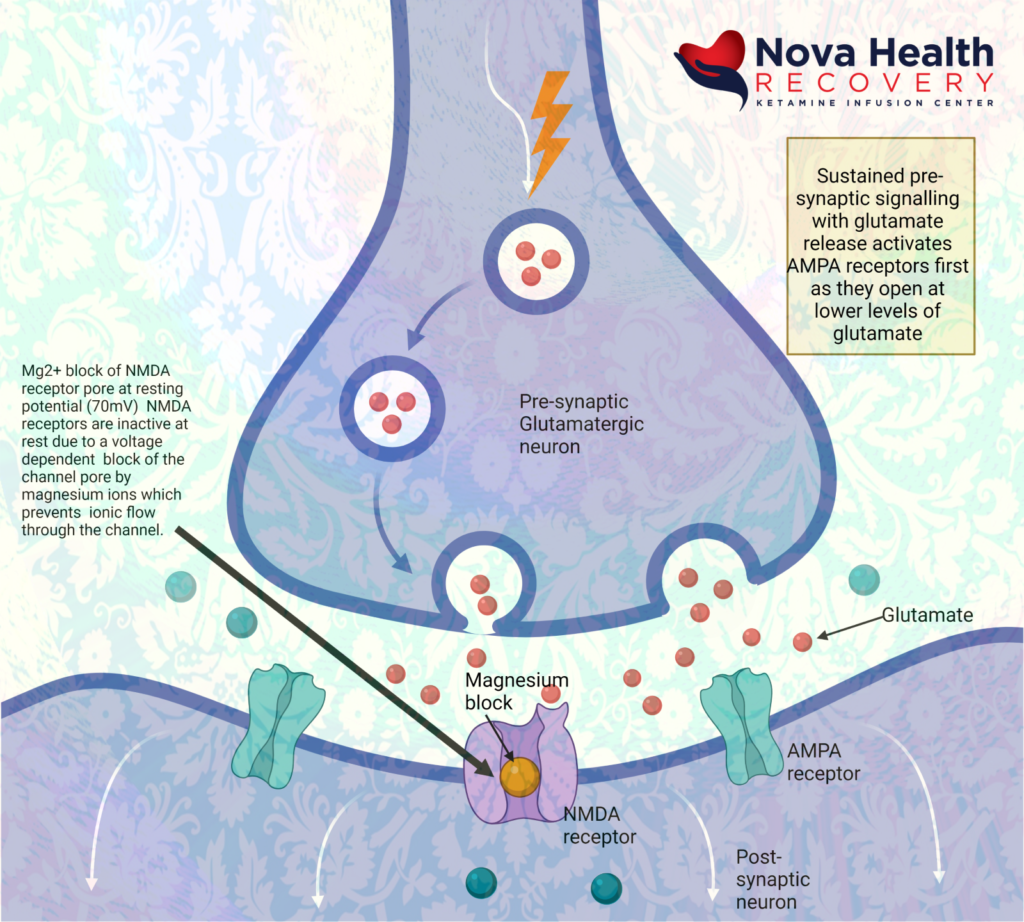
- AMPA receptors open due to binding with glutamate, letting in sodium to depolarize post-synaptic neuron:
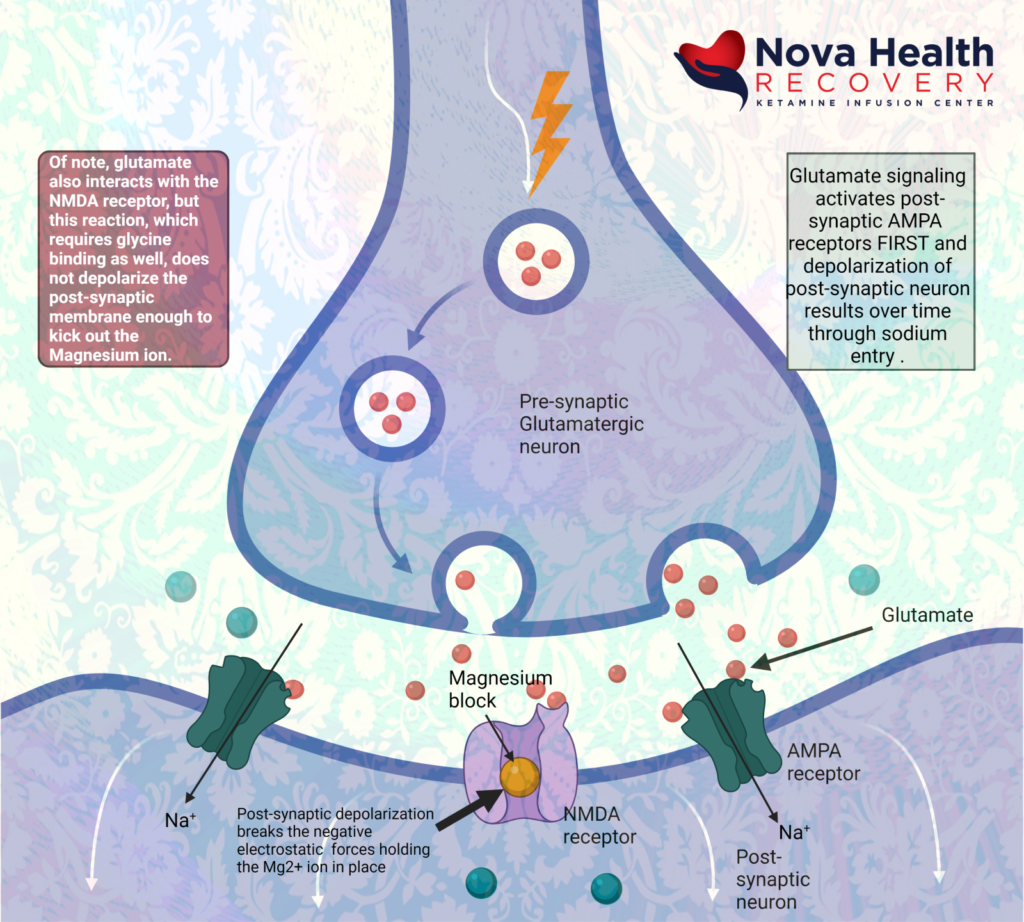
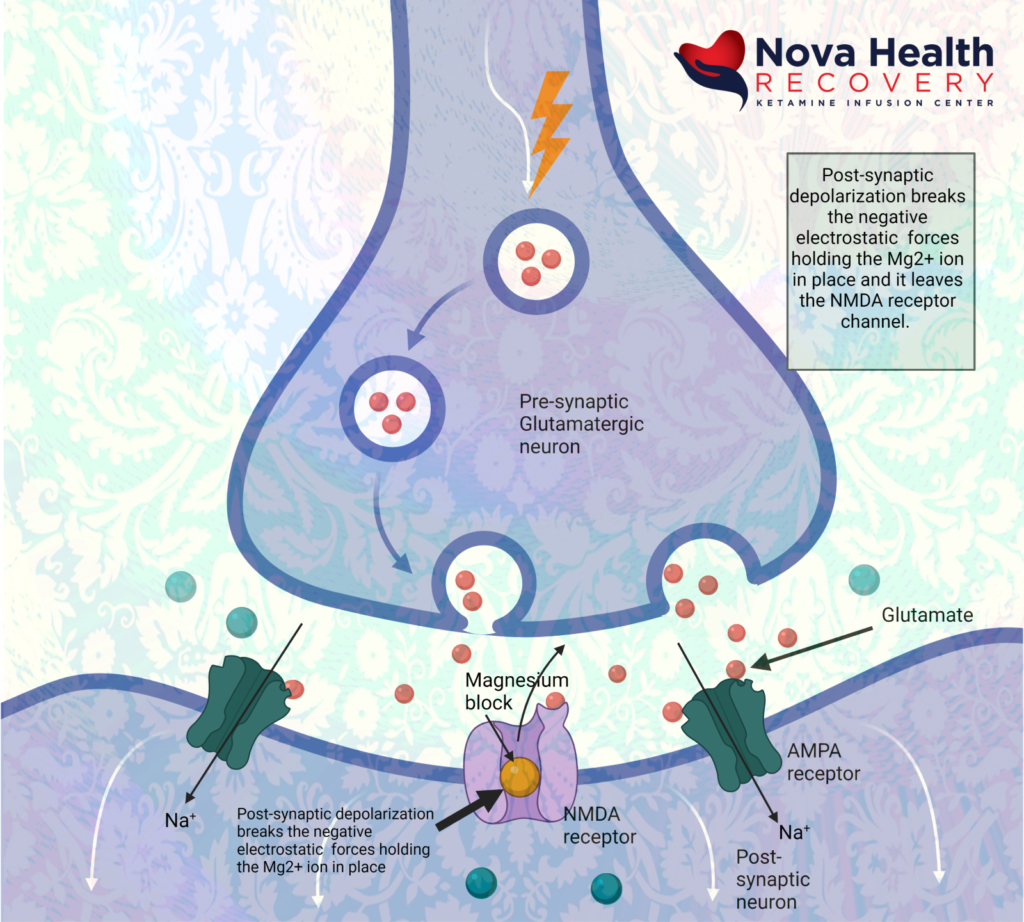
- Magnesium is extruded from the NMDA receptor pore due to depolarization of post-synaptic neuron. Calcium and sodium can enter through the receptor pore now causing metabolic signaling:
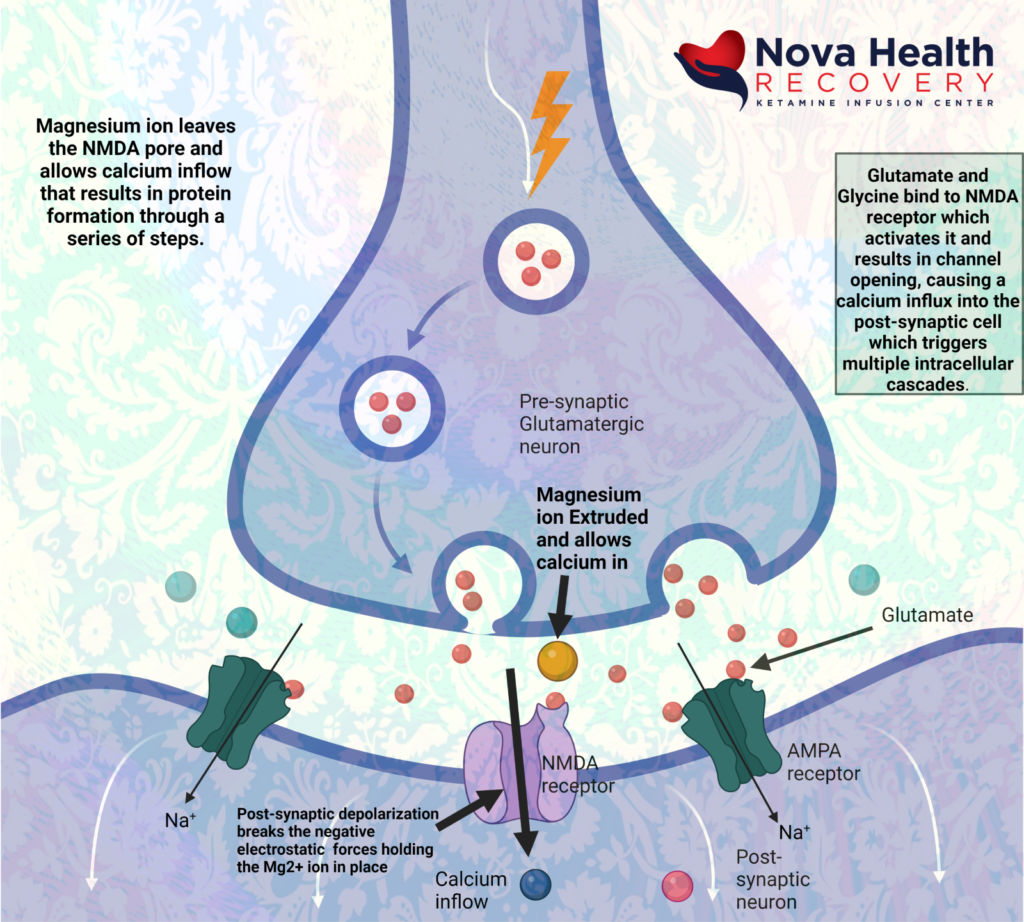
Ketamine acts at the internal pore PCP site in the intracellular portion of the pore, where it’s binding primarily on the Glu2N unit results in the decreased opening time of the pore and less calcium inflow. This decreases sensory input to higher areas of the CNS, such as emotional response, learning and memory.
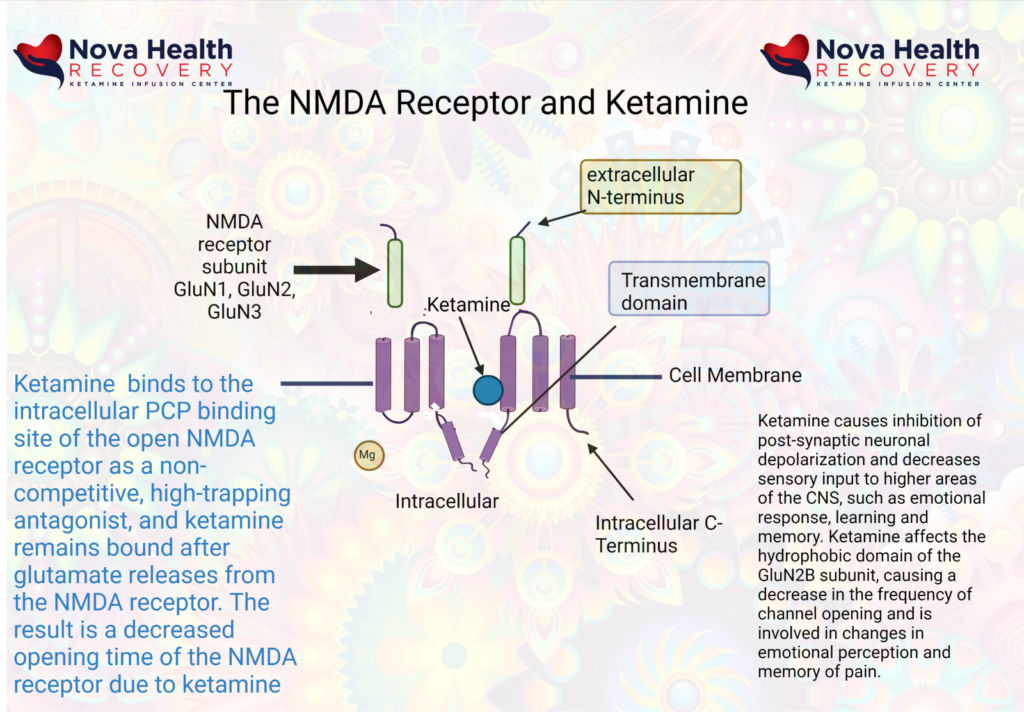
As a result of ketamine’s actions in altering excessive NMDA receptor activation, emotional and pain signaling are modified. Learning and memory may be modified through ketamine’s effects on the hippocampus, and there is enhanced emotional control as the PFC gains control over the limbic brain.
Ketamine has dissociative properties:
Sub-anesthetic doses of ketamine can produce states characterized by hallucinations, feelings of detachment from the environment, delirium, feelings of detachment from self, agitation, visual and auditory distortions all of which are characteristic of a dissociative state. Blood levels of ketamine are generally between 50-100 ng/ml. This state is due to blocking of the NMDA channel by ketamine with dysregulated excitatory neuronal activity. In this state of dissociation, one will find excessive glutamate release, increased dopamine activity, altered synaptic homeostasis, and decreased acetylcholine activity.
Dissociation is a state in which sensory inputs can reach the cerebral cortex but are not perceived in processing areas.
Ketamine and pain management:
Ketamine therapy causes alterations in gene expression and cell signaling that interrupt pathological changes associated with chronic pain. These include:
- Increased concentration of amines (5HT, NA, DA) which increases downward inhibition of pain perception
- Changes the NMDA receptor expression which is altered (by phosphorylation) in chronic pain states
- Ketamine acts as an anti-inflammatory agent and can downregulate activated astrocytes that may be producing inflammatory changes present in chronic pain
- Increased synaptic plasticity (neuroplasticity)
- Ketamine modifies opioid receptor responsivity
- Inhibition of nitric oxide synthase
Ketamine may improve neuropathic pain, in part, by decreasing depression seen in neuropathic pain. The neurological signals for pain do run alongside pathways involved in mood. Emotional pain and physical pain are interrelated. (9)
Ketamine and its antidepressant effects
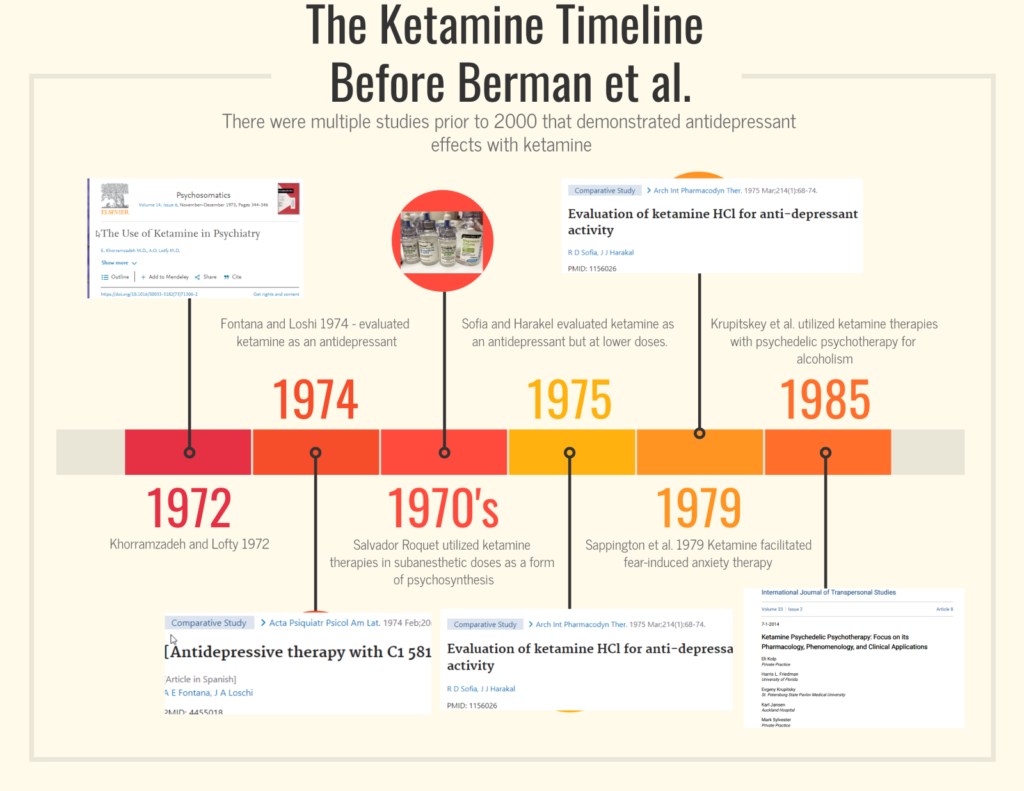
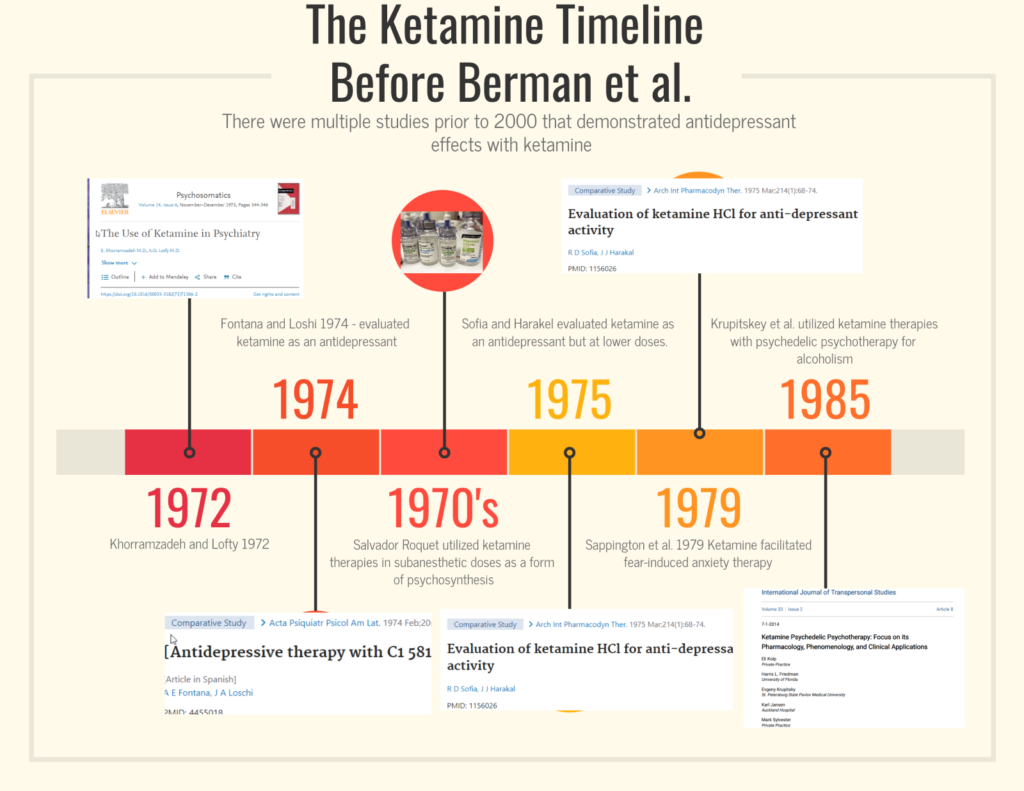
Although ketamine was discovered in 1962 and FDA approved for anesthesia in 1970, ketamine was quickly recognized as having the potential to augment psychotherapy. the earliest studies were in 1972 in Iran as listed above in the timeline. It wasn’t until the year 2000 when Berman et al. did a small study of ketamine in treatment-resistant cases that demonstrated the rapid and robust efficacy of ketamine therapy.
At low doses of ketamine, there is a rebalancing of glutamatergic activity and GABA levels due to alterations in intracellular cascades set off by the ketamine therapy. As a simplified level, high levels of glutamate and low GABA levels can lead to anxiety. High levels of glutamate are toxic to neurons. On the other hand, depleted glutamate levels can contribute to depression.
Treatment of depression with ketamine therapy sets off a cascade of interlocking systems. Blocking NMDA receptors at inhibitory interneurons in the brain results in a decreased functioning of GABA neurons that allows for increased activity at specific synapses. The blockage of these interneurons is a ‘go’ signal for the rapid release of glutamate at the synapse, which activates the postsynaptic neuron to produce proteins that allow for increased neural plasticity.
The rapid increase of glutamate in the synapse initially activates AMPA receptors, which results in a calcium influx that depolarizes the neuron. There is a resulting cascade of metabolism that results in the stimulation and formation of brain-derived neurotrophic factor (BDNF) and the mTOR pathways. This results in increased synapse formation, increased synaptic strength, and alterations in neurotransmitter control, especially of serotonin and dopamine. The promotion of synaptic growth can “reset” the stress that has caused structural changes in depression. This allows for improved emotional processing as well as improved functioning of memory areas, the prefrontal cortex ( executive functioning), and the hippocampus (short-term memory).
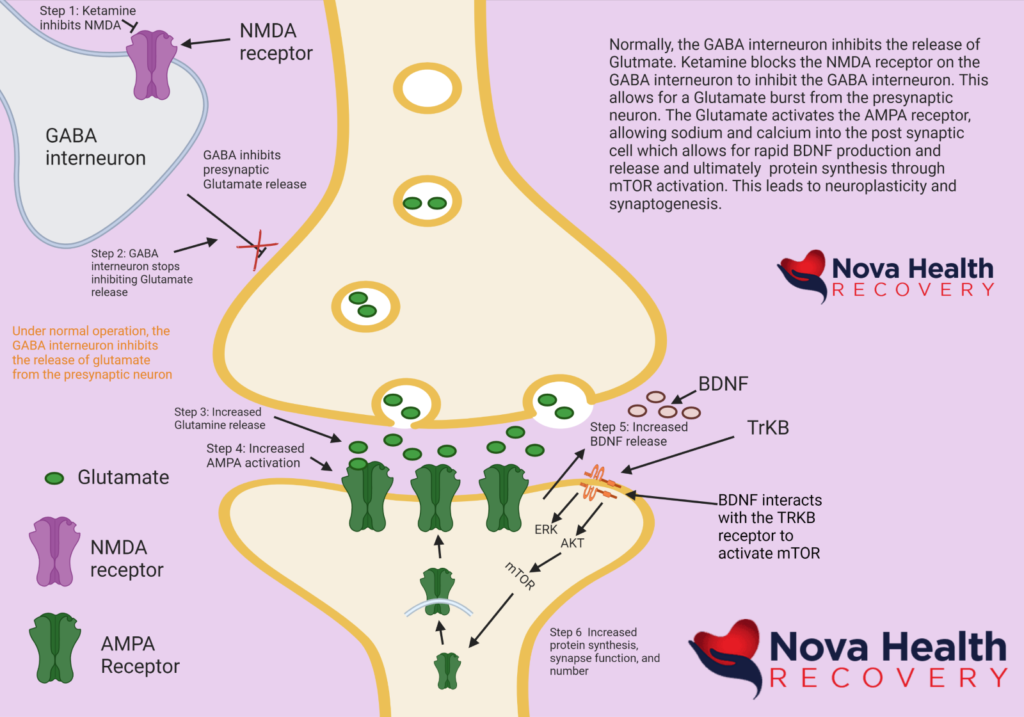
What makes ketamine therapy unique is that it is affecting the glutamatergic system. Looking at the diagram above, in review, the following sequence of events occurs:
- Ketamine binds to the NMDA receptor on the GABA interneuron. This blocks the NMDA receptor and turns off the GABA interneuron.
- The GABA interneuron stops inhibiting glutamate release at the synapse. This is a “go” signal for the release of glutamate from the presynaptic neuron.
- Glutamate is released into the synapse.
- Glutamate interacts with AMPA receptors, causing them to open and allow in sodium, thereby depolarizing the postsynaptic neuron. Generally, excess glutamate is taken up by astrocytes that are part of the synapse. The excess glutamate is converted to glutamine in the astrocytes and then sent back to the presynaptic neuron where it is converted back to glutamate to be reused again. Glutamate can be converted into GABA as well.
- BDNF is released from vesicles and interacts with tyrosine kinase B (TrKB) which then sets off more intracellular cascades to activate mTOR, which results in the production of proteins leading to synapse formation.
What are the risks of ketamine use?
Ketamine is one of the safest drugs available because of its ability to maintain cardiovascular status with minimal support. The World Health Organization has had ketamine on its essential medicines list since 1985. Most cases of death associated with ketamine use are in conjunction with either significant medical conditions or other drug use. Ketamine can certainly be misused and abused, but it has no physiological withdrawal. There could certainly be some psychological dependence, however, if ketamine therapy has effectively made a person less depressed, depression may return after ketamine therapies are stopped. It is of note that when ketamine is used as an antidepressant, the antidepressant effects last way beyond the presence of ketamine in the system. It is not the psychedelic effect of ketamine that is producing the antidepressant effect, but rather the neural plasticity that follows.
Ketamine produces different responses in patients who are depressed versus individuals who are not depressed. Most abuse of ketamine occurs in the context of other drug use in individuals who have no depression, but rather use ketamine for pleasure. One must be careful in the context of the fentanyl epidemic not to accidentally ingest fake ketamine and end up with an overdose of fentanyl. The other issue with snorting ketamine off the street is that it is generally higher doses and anesthetic in nature. Anesthetic doses are not antidepressants as they affect different systems in the brain.
In monitored settings, ketamine is extremely safe, especially in the treatment of mood disorders where the doses are less than 1/10 of what would be used for anesthetic purposes.
There can be changes in heart rate, with an increase in heart rate, as well as blood pressure increases transiently during treatment with ketamine therapy. Other short-term side effects during ketamine therapy include nausea, vomiting, nystagmus, loss of balance, altered states of consciousness, confusion, and sedation.
Ultra-high doses of ketamine that are used to poison rats in controlled studies and in study cases of ketamine abuse as seen in Southeast Asia at grams per day over many months demonstrate the possibility for bladder issues, stomach pain, and alterations of mood. This type of abuse is rarely seen in the United States.
Ketamine Assisted Psychotherapy
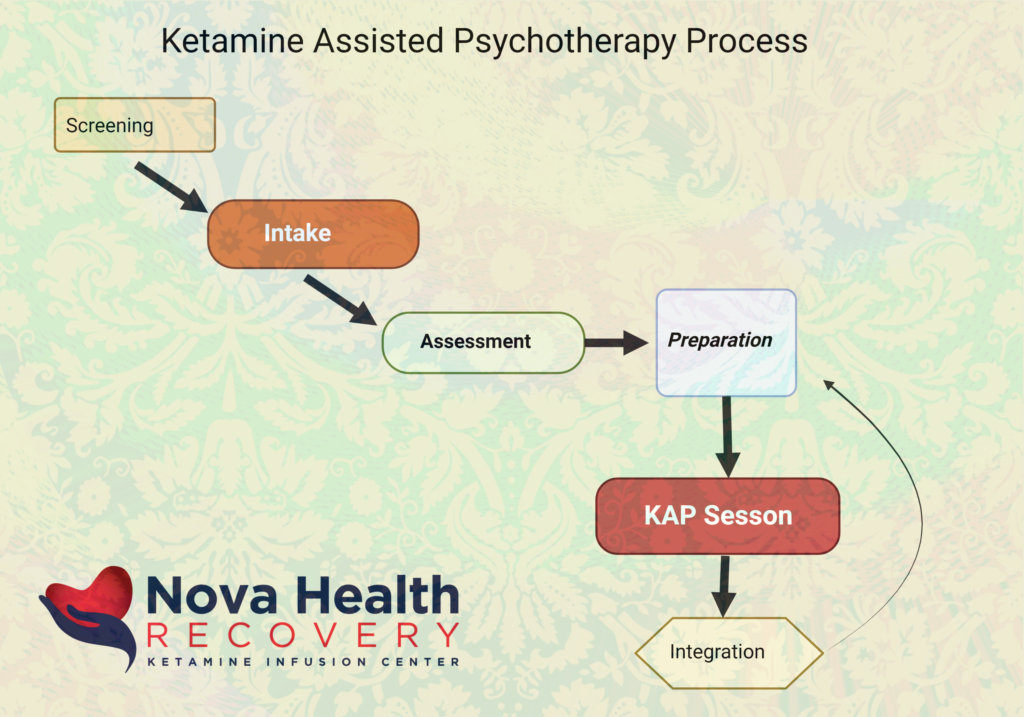
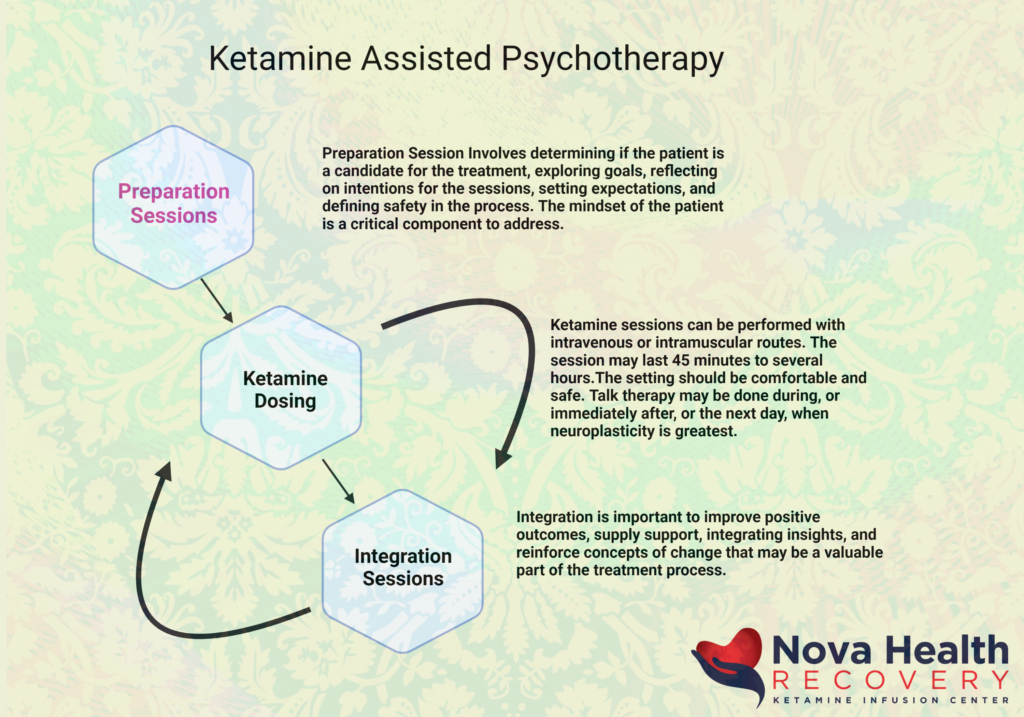
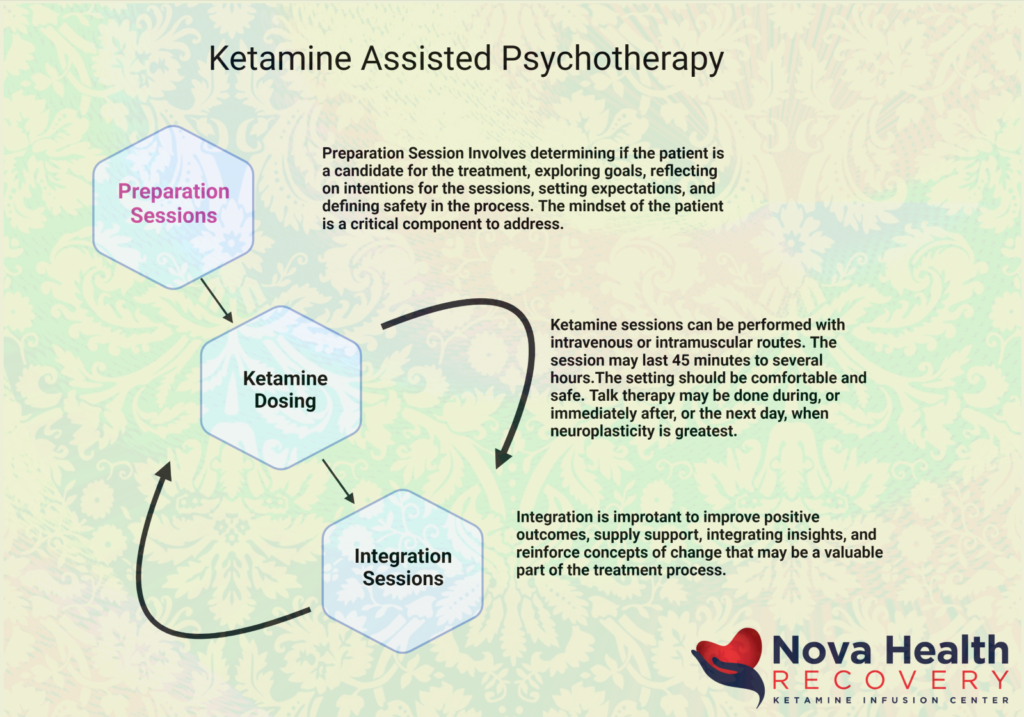
Ketamine has been used in the treatment of mood disorders with great efficacy and robust effects. 70% of patients with treatment resistant depression may have significant improvement or remission by the third infusion out of six that are generally given over two weeks. The combination of ketamine therapy with psychotherapy provides a stronger construct for the maintenance of effect with ketamine treatment. The evidence-based medicine behind KAP is explored in another article, but generally there are preparatory sessions, in which the person’s eligibility for treatment is defined and establishing treatment goals and expectations. The person then receives, at a later time, the ketamine dosing, whether it is by intravenous or intramuscular approaches, with sessions lasting between 45 minutes to several hours in length. Psychotherapy sessions can be applied during the ketamine experience or immediately after as an integration. Subsequent integration therapy is critical when the person has returned from their altered states of consciousness in order to focus on positive outcomes, supply support, integrating insights, and reinforcing concepts of change that may be a valuable part of the treatment process.
1 Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018 Apr;23(4):801-811. doi: 10.1038/mp.2017.255. Epub 2018 Mar 13. PMID: 29532791; PMCID: PMC5999402.
2. Muller J, Pentyala S, Dilger J, Pentyala S. Ketamine enantiomers in the rapid and sustained antidepressant effects. Ther Adv Psychopharmacol. 2016 Jun;6(3):185-92. doi: 10.1177/2045125316631267. Epub 2016 Mar 10. PMID: 27354907; PMCID: PMC4910398.
3 Jelen LA, Young AH, Stone JM. Ketamine: A tale of two enantiomers. J Psychopharmacol. 2021 Feb;35(2):109-123. doi: 10.1177/0269881120959644. Epub 2020 Nov 6. PMID: 33155503; PMCID: PMC7859674.
4 Yang C, Shirayama Y, Zhang JC, Ren Q, Yao W, Ma M, Dong C, Hashimoto K. R-ketamine: a rapid-onset and sustained antidepressant without psychotomimetic side effects. Transl Psychiatry. 2015 Sep 1;5(9):e632. doi: 10.1038/tp.2015.136. Erratum in: Transl Psychiatry. 2020 Aug 21;10(1):295. PMID: 26327690; PMCID: PMC5068814.
5 Zhang JC, Li SX, Hashimoto K. R (-)-ketamine shows greater potency and longer lasting antidepressant effects than S (+)-ketamine. Pharmacol Biochem Behav. 2014 Jan;116:137-41. doi: 10.1016/j.pbb.2013.11.033. Epub 2013 Dec 3. PMID: 24316345.
6 Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature. 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355; PMCID: PMC4922311.
7 Hashimoto K. Molecular mechanisms of the rapid-acting and long-lasting antidepressant actions of (R)-ketamine. Biochem Pharmacol. 2020 Jul;177:113935. doi: 10.1016/j.bcp.2020.113935. Epub 2020 Mar 26. PMID: 32224141.
8 Sarton E, Teppema LJ, Olievier C, Nieuwenhuijs D, Matthes HW, Kieffer BL, Dahan A. The involvement of the mu-opioid receptor in ketamine-induced respiratory depression and antinociception. Anesth Analg. 2001 Dec;93(6):1495-500, table of contents. doi: 10.1097/00000539-200112000-00031. PMID: 11726430.
9. Wang J, Goffer Y, Xu D, Tukey DS, Shamir DB, Eberle SE, Zou AH, Blanck TJ, Ziff EB. A single subanesthetic dose of ketamine relieves depression-like behaviors induced by neuropathic pain in rats. Anesthesiology. 2011 Oct;115(4):812-21. doi: 10.1097/ALN.0b013e31822f16ae. PMID: 21934410; PMCID: PMC3222930.
The Narrative of Ketamine-Assisted-Psychotherapy and Why It Works
The Narrative of Ketamine-Assisted-Psychotherapy and Why It Works
A systematic narrative review on ketamine-assisted psychotherapy (KAP) by SJ Drozdz et al (2022) discusses practices currently in place with 17 articles and 603 participants identified. The conclusion of the paper is that combined treatments of ketamine therapies with psychotherapy (KAP) can initiate and prolong clinically significant reductions in pain, anxiety, and depressive symptoms.
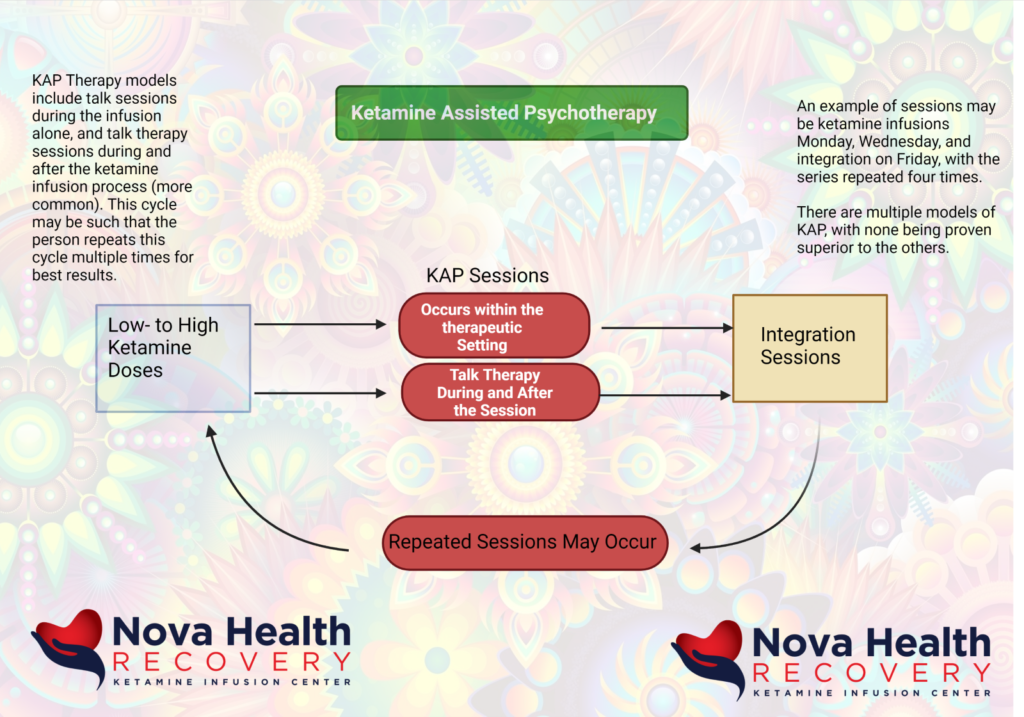
There are multiple variations in which KAP is applied, such as the dose, frequency, route of ketamine given, as well as the psychotherapy modality used, and overall treatment length. The findings of this review demonstrated that psychotherapy provided before, during, and after ketamine sessions can maximize and prolong benefits.
The STAR*D trial demonstrated the low response rates to new antidepressants after the failure of the first antidepressant, the delay in onset of efficacy, and the high rates of relapse in patients with depression. The prevalence of major depressive disorder is 6.4% in the US population, and there are few medications with novel mechanisms of action that have been developed over the past six decades. This is one of the reasons why ketamine and therapies associated with it have gained interest. They are rapid in onset, highly effective, but have poor sustained benefit. This requires repeat dosing if there are no other therapies added.
Ketamine was created in 1962 and is utilized not just as an anesthetic agent but also for mental health purposes. The manners with which ketamine works include:
- Alterations in brain circuit functioning
- Enhanced synaptogenesis ( formation of new synapses between neurons)
- Glutamate modulation
- Increased neural plasticity
Ketamine is primarily an NMDA receptor antagonist which suppresses a tonically active form of glutamatergic signaling in the brain.(1) Ketamine activates multiple signal cascades that include mammalian target of rapamycin (mTOR), inhibition of glycogen synthase kinase-3 (GSK-3), and elongation factor 2 kinase (eEF2) which results in increased neural plasticity. (1) (2) (3) (4) (5) This is accomplished when ketamine suppresses GABA-ergic interneurons that leads to decreased inhibition at the synapse and results in a brief excitation and release of glutamine at the synapse. (1) The brief resulting synaptic excitation results in structural neuronal plasticity and plays a significant role in ketamine’s robust and rapid effectiveness in substance use disorders, chronic pain, and mental health conditions. (5) (6)(7) The only problem with this treatment is that results may only last between four and seven days and may require multiple treatments to maintain the effects. (8)(9)
It is the short duration of ketamine therapy’s effect that has resulted in a search for methods to prolong its antidepressant effects. Psychotherapy is one method to promote the effective lengthening of ketamine’s results. Psychotherapy is a treatment of psychological disorders through the promotion of personal growth, symptom management, and wellness that is based on therapeutic principles, structures, and techniques. (10)
Ketamine was used to facilitate psychotherapy as early as 1973 by Khorramzadeh and Lotfy in which it was used as an abreactive agent. (11) Ketamine was subsequently used in antidepressant psychotherapy with Fontana in 1974.(12)
Ketamine enhanced psychotherapy has been used for several different conditions which include:
- Opioid tapering (13)
- Neuropathic pain (14)
- Major depressive disorder, generalized anxiety disorder, ADHD, obsessive-compulsive disorder, substance use disorder, and PTSD. (15)
Ketamine can facilitate emotional learning through its effects on neural plasticity as well as its emotional arousing phenomenological experiences. Ketamine can reduce defensiveness and increase engagement and treatment adherence of patients. (16,17,18, 19, 20) The psychedelic experiences of ketamine allows an individual to have new perspective with critical reframing of their situation as well as gaining personal insights of themselves. The therapist as well can gain further insight into the patient as the individual begins to have more cognitive flexibility. It is through conscious awareness that ketamine may be augmenting the effects of psychotherapy.(15) This may also play a role in ketamine’s effectiveness in addiction disorders.(21) (22)
The mechanism by which ketamine improves psychotherapy is based on the increased access to traumatic memories through altered synaptic connections, down-regulation of our prefrontal cortex resulting in decreased central sensitization, and alterations of previously paired pain-related memories.(23) For ketamine-assisted psychotherapy, ketamine doses can be escalated to allow various altered states of consciousness including out-of-body experiences.
There are multiple studies utilizing ketamine with various psychotherapies. Ketamine has been administered in numerous formats including intravenously, intramuscularly, intranasally, and orally at varying doses. The setting in many of the studies was not described as well. The timing of psychotherapies also varied among different trials and included psychotherapy before, during, and after ketamine infusions with varying permutations of this. Among the psychotherapy types administered, cognitive behavioral therapy, mindfulness-based interventions, and motivational enhancement therapy were among the modalities used. Action and commitment therapy also may have effectiveness when utilized with ketamine treatments.
This systematic review by SJ Drozdz et al (2022) demonstrated that ketamine assisted psychotherapy can be effective to initiate rapid, significant benefits for a wide range of disorders, however many of the studies were quite variable. There have been multiple studies demonstrating KAP efficacy in the treatment of anxiety and depression. (15, 24, 25, 26, 27, 28,29,30)
The use of KAP allows for treatment engagement (20) and this allows for rapid reduction in depression and anxiety and lower dropout rates with increase participation in therapy. (31) The psychoactive properties of high ketamine doses increase psychedelic experiences, which reduce defensiveness, increase rapport, and increase transpersonal experiences to improve decision-making and inner healing, which is been observed in PTSD, addiction and depression. (15, 20, 32, 33)
The neural plasticity that results from ketamine therapy also helps with fear extinction, restructuring of traumatic memories, and new memory formation. (5)
Common themes that were found to be more effective in Therapy include:
- Preparation of patients with goal setting and positive expectations to promote therapeutic alliance (15,20,32)
- Supervision by qualified personnel during ketamine fusions to help guide transformational experiences, provide comfort during times of distress, and evoke psychological insight
- Psychotherapy should additionally be provided after the infusion to allow integration of transpersonal experiences from the treatment and promote insights discovered during so that they are fully accepted.
- Longer-term psychotherapy may be of value.
Multiple doses of ketamine over multiple sessions may provide better efficacy. This has been seen in sessions with cannabis users (34) in which non-responders and those with difficulty in maintaining abstinence responded to multiple KAP Sessions. The same is seen with heroin users, in which multiple doses maintain greater abstinence rates than those given a single dose. (27) Likewise, multiple administrations can prolong therapeutic effects and can convert non-responders into responders.(27, 28) In heroin users, higher doses of ketamine with psychotherapy may also increase durability of gains and heroin abstinence compared to lower doses. (33)
in summary, higher doses of ketamine, more frequent KAP sessions, and longer durations of psychotherapy will increase the efficacy and durability of improvements in multiple disorders.(15, 34, 35) The exact treatment paradigm chosen has yet to be revealed as studies are variable, but these are merely guidelines that seem to demonstrate efficacy. As far as non-responders are concerned, they may require additional ketamine sessions or perhaps a higher dose to achieve response. (27, 34)
The use of ketamine assisted psychotherapy in pain related concerns has not been studied well. There is interaction with mental health, pain, and addictive disorders, so there is a high level of comorbidity with mutual exacerbation of symptoms. (36, 37,38) Patients with chronic pain are two to three times more likely to experience anxiety disorders. (39, 40, 41). 20 to 50% of chronic pain patients have comorbid depression. (42,43,44) . 36 to 56% of patients with chronic pain experience substance use disorder in their lifetime. (45) Patients with pain conditions will more likely develop mental health and addictive disorders, and those with depression are more likely to develop addictive and/or pain conditions. (45,46,47)
Psychotherapy can be effective in the treatment of pain, (48,49,50) but psychotherapy is not enough to manage pain. Given the interaction of the experience of pain, mental health, and substance abuse, outcomes are better when all comorbid conditions are treated concurrently. (51,52).
Trials Used that incorporated ketamine with psychotherapy:
Case Reports:
21. Keizer BM, Roache JD, Jones JR, Kalpinski RJ, Porcerelli JH, Krystal JH. Continuous ketamine infusion for pain as an opportunity for psychotherapy for PTSD: a case series of ketamine-enhanced psychotherapy for PTSD and pain (KEP-P2). Psychother Psychosom. 2020;89(5):326–329. doi:10.1159/000507095
22. Ocker AC, Shah NB, Schwenk ES, Witkowski TA, Cohen MJ, Viscusi ER. Ketamine and cognitive behavioral therapy for rapid opioid tapering with sustained opioid abstinence: a case report and 1‐year follow‐up. Pain Pract. 2020;20(1):95–100. doi:10.1111/papr.12829
28. Becker J. Regarding the transpersonal nature of ketamine therapy: an approach to the work. Int J Transpers Stud. 2014;33(2):151–159. doi:10.24972/ijts.2014.33.2.151
36. Adams TG, Bloch MH, Pittenger C. Intranasal ketamine and cognitive-behavioral therapy for treatment-refractory obsessive-compulsive disorder. J Clin Psychopharmacol. 2017;37(2):269–271. doi:10.1097/JCP.0000000000000659
Two Pilot Trials:
38. Pradhan B, Mitrev L, Moaddell R, Wainer IW. d -Serine is a potential biomarker for clinical response in treatment of post-traumatic stress disorder using (R, S)-ketamine infusion and TIMBER psychotherapy: a pilot study. Biochimica et Biophysica Acta. 2018;1866(7):831–839. doi:10.1016/j.bbapap.2018.03.006
42. Dakwar E, Levin F, Hart CL, et al. A single ketamine infusion combined with motivational enhancement therapy for alcohol use disorder: a randomized midazolam-controlled pilot trial. Am J Psychiatr. 2020;177(2):125–133. doi:10.1176/appi.ajp.2019.19070684
Proof-of-concept trials:
41. Shiroma PR, Thuras P, Wels J, Erbes C, Kehle-Forbes S, Polusny M. A proof-of-concept study of subanesthetic intravenous ketamine combined with prolonged exposure therapy among veterans with posttraumatic stress disorder. J Clin Psychiatry. 2020;81(6). doi:10.4088/JCP.20l13406
46. Azhari N, Hu H, O’Malley KY, Blocker ME, Levin FR, Dakwar E. Ketamine-facilitated behavioral treatment for cannabis use disorder: a proof-of-concept study. Am J Drug Alcohol Abuse. 2021;47(1):92–97. doi:10.1080/00952990.2020.1808982
References:
1 Kavalali ET, Monteggia LM. Synaptic mechanisms underlying rapid antidepressant action of ketamine. Am J Psychiatr. 2012;169(11):1150–1156. doi:10.1176/appi.ajp.2012.12040531
2 Maeng S, Zarate CA, Du J, et al. Cellular mechanisms underlying the antidepressant effects of ketamine: role of α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptors. Biol Psychiatry. 2008;63(4):349–352. doi:10.1016/j.biopsych.2007.05.028
3 Zanos P, Moaddel R, Morris PJ, et al. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature. 2016;533(7604):481–486. doi:10.1038/nature17998
4 Zunszain PA, Horowitz MA, Cattaneo A, Lupi MM, Pariante CM. Ketamine: synaptogenesis, immunomodulation and glycogen synthase kinase-3 as underlying mechanisms of its antidepressant properties. Mol Psychiatry. 2013;18(12):1236–1241. doi:10.1038/mp.2013.87
5 Collo G, Pich E. Ketamine enhances structural plasticity in human dopaminergic neurons: possible relevance for treatment-resistant depression. Neural Regener Res. 2018;13(4):645. doi:10.4103/1673-5374.230288
6 Iadarola ND, Niciu MJ, Richards EM, et al. Ketamine and other N-methyl-D-aspartate receptor antagonists in the treatment of depression: a perspective review. Ther Adv Chronic Dis. 2015;6(3):97–114. doi:10.1177/2040622315579059
7 Dakwar E, Levin F, Foltin RW, Nunes EV, Hart CL. The effects of subanesthetic ketamine infusions on motivation to quit and cue-induced craving in cocaine-dependent research volunteers. Biol Psychiatry. 2014;76(1):40–46. doi:10.1016/j.biopsych.2013.08.009
8 Murrough JW, Iosifescu DV, Chang LC, et al. Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatr. 2013;170(10):1134–1142. doi:10.1176/appi.ajp.2013.13030392
9 Feder A, Parides MK, Murrough JW, et al. Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder. JAMA Psychiatr. 2014;71(6):681. doi:10.1001/jamapsychiatry.2014.62
10 Cuijpers P. Four decades of outcome research on psychotherapies for adult depression: an overview of a series of meta-analyses. Can Psychol. 2017;58(1):7–19. doi:10.1037/cap0000096
11 Khorramzadeh E, Lotfy AO. The use of ketamine in psychiatry. Psychosomatics. 1973;14(6):344–346. doi:10.1016/S0033-3182(73)71306-2
12 Fontana AE, Loschi JA. [Antidepressive therapy with C1 581]. Acta Psiquiatr Psicol Am Lat. 1974;20(1):32–39. Catalan.
13 Ocker AC, Shah NB, Schwenk ES, Witkowski TA, Cohen MJ, Viscusi ER. Ketamine and cognitive behavioral therapy for rapid opioid tapering with sustained opioid abstinence: a case report and 1‐year follow‐up. Pain Pract. 2020;20(1):95–100. doi:10.1111/papr.12829
14 Keizer BM, Roache JD, Jones JR, Kalpinski RJ, Porcerelli JH, Krystal JH. Continuous ketamine infusion for pain as an opportunity for psychotherapy for PTSD: a case series of ketamine-enhanced psychotherapy for PTSD and pain (KEP-P2). Psychother Psychosom. 2020;89(5):326–329. doi:10.1159/000507095
15 Dore J, Turnipseed B, Dwyer S, et al. Ketamine Assisted Psychotherapy (KAP): patient demographics, clinical data and outcomes in three large practices administering ketamine with psychotherapy. J Psychoactive Drugs. 2019;51(2):189–198. doi:10.1080/02791072.2019.1587556
16 Myers KM, Carlezon WA, Davis M. Glutamate receptors in extinction and extinction-based therapies for psychiatric illness. Neuropsychopharmacology. 2011;36(1):274–293. doi:10.1038/npp.2010.88
17 Dakwar E, Anerella C, Hart CL, Levin FR, Mathew SJ, Nunes EV. Therapeutic infusions of ketamine: do the psychoactive effects matter? Drug Alcohol Depend. 2014;136:153–157. doi:10.1016/j.drugalcdep.2013.12.019
18 Dakwar E, Nunes EV, Hart CL, Hu MC, Foltin RW, Levin FR. A sub-set of psychoactive effects may be critical to the behavioral impact of ketamine on cocaine use disorder: results from a randomized, controlled laboratory study. Neuropharmacology. 2018;142:270–276. doi:10.1016/j.neuropharm.2018.01.005
19 Luckenbaugh DA, Niciu MJ, Ionescu DF, et al. Do the dissociative side effects of ketamine mediate its antidepressant effects? J Affect Disord. 2014;159:56–61. doi:10.1016/j.jad.2014.02.017
20 Becker J. Regarding the transpersonal nature of ketamine therapy: an approach to the work. Int J Transpers Stud. 2014;33(2):151–159. doi:10.24972/ijts.2014.33.2.151
21 Ivan Ezquerra-Romano I, Lawn W, Krupitsky E, Morgan CJA. Ketamine for the treatment of addiction: evidence and potential mechanisms. Neuropharmacology. 2018;142:72–82. doi:10.1016/j.neuropharm.2018.01.017
22 Krupitsky EM, Grinenko AY. Ketamine Psychedelic Therapy (KPT): a review of the results of ten years of research. J Psychoactive Drugs. 1997;29(2):165–183. doi:10.1080/02791072.1997.10400185
(23) Keizer BM, Roache JD, Jones JR, Kalpinski RJ, Porcerelli JH, Krystal JH. Continuous ketamine infusion for pain as an opportunity for psychotherapy for PTSD: a case series of ketamine-enhanced psychotherapy for PTSD and pain (KEP-P2). Psychother Psychosom. 2020;89(5):326–329. doi:10.1159/000507095
(24) Duek O, Kelmendi B, Pietrzak RH, Harpaz-Rotem I. Augmenting the Treatment of PTSD with Ketamine—a Review. Curr Treat Options Psychiatr. 2019;6(2):143–153. doi:10.1007/s40501-019-00172-0
25 Halstead M, Reed S, Krause R, Williams MT. Ketamine-assisted psychotherapy for PTSD related to racial discrimination. Clin Case Stud. 2021;20(4):310–330. doi:10.1177/1534650121990894
26 Shiroma PR, Thuras P, Wels J, Erbes C, Kehle-Forbes S, Polusny M. A proof-of-concept study of subanesthetic intravenous ketamine combined with prolonged exposure therapy among veterans with posttraumatic stress disorder. J Clin Psychiatry. 2020;81(6). doi:10.4088/JCP.20l13406
27 Krupitsky EM, Burakov AM, Dunaevsky IV, Romanova TN, Slavina TY, Grinenko AY. Single versus repeated sessions of ketamine-assisted psychotherapy for people with heroin dependence. J Psychoactive Drugs. 2007;39(1):13–19. doi:10.1080/02791072.2007.10399860
28 Wilkinson ST, Wright D, Fasula MK, et al. Cognitive behavior therapy may sustain antidepressant effects of intravenous ketamine in treatment-resistant depression. Psychother Psychosom. 2017;86(3):162–167. doi:10.1159/000457960
29 Wilkinson ST, Rhee TG, Joormann J, et al. Cognitive behavioral therapy to sustain the antidepressant effects of ketamine in treatment-resistant depression: a randomized clinical trial. Psychother Psychosom. 2021;90(5):318–327. doi:10.1159/000517074
30 Adams TG, Bloch MH, Pittenger C. Intranasal ketamine and cognitive-behavioral therapy for treatment-refractory obsessive-compulsive disorder. J Clin Psychopharmacol. 2017;37(2):269–271. doi:10.1097/JCP.0000000000000659
31 Aderka IM, Nickerson A, Bøe HJ, Hofmann SG. Sudden gains during psychological treatments of anxiety and depression: a meta-analysis. J Consult Clin Psychol. 2012;80(1):93–101. doi:10.1037/a0026455
32 Halstead M, Reed S, Krause R, Williams MT. Ketamine-assisted psychotherapy for PTSD related to racial discrimination. Clin Case Stud. 2021;20(4):310–330. doi:10.1177/1534650121990894
33 Krupitsky E, Burakov A, Romanova T, Dunaevsky I, Strassman R, Grinenko A. Ketamine psychotherapy for heroin addiction: immediate effects and two-year follow-up. J Subst Abuse Treat. 2002;23(4):273–283. doi:10.1016/S0740-5472(02)00275-1
34 Azhari N, Hu H, O’Malley KY, Blocker ME, Levin FR, Dakwar E. Ketamine-facilitated behavioral treatment for cannabis use disorder: a proof of concept study. Am J Drug Alcohol Abuse. 2021;47(1):92–97. doi:10.1080/00952990.2020.1808982
35 Krupitsky E, Burakov A, Romanova T, Dunaevsky I, Strassman R, Grinenko A. Ketamine psychotherapy for heroin addiction: immediate effects and two-year follow-up. J Subst Abuse Treat. 2002;23(4):273–283. doi:10.1016/S0740-5472(02)00275-1
36 Gallagher RM, Verma S. Managing pain and comorbid depression: a public health challenge. Semin Clin Neuropsychiatry. 1999;4(3):203–220.
37 Blier P, Abbott FV. Putative mechanisms of action of antidepressant drugs in affective and anxiety disorders and pain. J Psychiatry Neurosci. 2001;26(1):37–43.
38 Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011;12(9):964–973. doi:10.1016/j.jpain.2011.03.003
39 Asmundson GJG, Katz J. Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety. 2009;26(10):888–901. doi:10.1002/da.20600
40 Katz J, Pagé MG, Fashler S, Rosenbloom BN, Asmundson GJG. Chronic pain and the anxiety disorders: epidemiology, mechanisms and models of comorbidity, and treatment. In: Mental Health and Pain. Paris: Springer; 2014:119–155. doi:10.1007/978-2-8178-0414-9_8
41 Demyttenaere K, Bruffaerts R, Lee S, et al. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain. 2007;129(3):332–342. doi:10.1016/j.pain.2007.01.022
42 Arnow BA, Hunkeler EM, Blasey CM, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68(2):262–268. doi:10.1097/01.psy.0000204851.15499.fc
43 Kroenke K. Somatic symptoms and depression: a double hurt. Prim Care Companion J Clin Psychiatr. 2005;07(04):148–149. doi:10.4088/PCC.v07n0401
44 Miller LR, Cano A. Comorbid chronic pain and depression: who is at risk? J Pain. 2009;10(6):619–627. doi:10.1016/j.jpain.2008.12.007
45 Martell BA, O’Connor PG, Kerns RD, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146(2):116. doi:10.7326/0003-4819-146-2-200701160-00006
46 Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry. 2003;60(1):39–47. doi:10.1001/archpsyc.60.1.39
47Croft PR, Papageorgiou AC, Ferry S, Thomas E, Jayson MI, Silman AJ. Psychologic distress and low back pain. Evidence from a prospective study in the general population. Spine. 1995;20(24):2731–2737. doi:10.1097/00007632-199512150-00015
48 Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999;80(1):1–13. doi:10.1016/S0304-3959(98)00255-3
49 van Tulder MW, Ostelo R, Vlaeyen JWS, Linton SJ, Morley SJ, Assendelft WJJ. Behavioral treatment for chronic low back pain. Spine. 2001;26(3):270–281. doi:10.1097/00007632-200102010-00012
50 Bogaards MC, ter Kuile MM. Treatment of recurrent tension headache: a meta-analytic review. Clin J Pain. 1994;10(3):174–190. doi:10.1097/00002508-199409000-00003
51 Castelnuovo G, Giusti EM, Manzoni GM, et al. Psychological treatments and psychotherapies in the neurorehabilitation of pain: evidences and recommendations from the Italian Consensus Conference on Pain in Neurorehabilitation. Front Psychol. 2016;7:115. doi:10.3389/fpsyg.2016.00115
52 Samwel HJA, Kraaimaat FW, Crul BJP, van Dongen RD, Evers AWM. Multidisciplinary allocation of chronic pain treatment: effects and cognitive-behavioural predictors of outcome. Br J Health Psychol. 2009;14(Pt 3):405–421. doi:10.1348/135910708X337760
53. Drozdz SJ, Goel A, McGarr MW, Katz J, Ritvo P, Mattina GF, Bhat V, Diep C, Ladha KS. Ketamine Assisted Psychotherapy: A Systematic Narrative Review of the Literature. J Pain Res. 2022 Jun 15;15:1691-1706. doi: 10.2147/JPR.S360733. PMID: 35734507; PMCID: PMC9207256.
What is Ketamine Assisted Psychotherapy and Studies That Used KAP
What is Ketamine Assisted Psychotherapy (KAP)? And Why KAP?
Ketamine was created in 1962, and FDA approved in 1974 and aesthetic purposes. Ketamine has been abused in certain party scenes, and it is known as “horse tranquilizer” and “special K” . Ketamine was also used in the Vietnam War because of its painkilling effects that did not impact respiratory or cardiovascular status. Of course, ketamine was used in veterinary work, but ketamine has been used in a wide variety of animals, not just horses.
Ketamine has been used in raves and electronic dance music festivals. The fear of many was that they would be knocked out by horse tranquilizer, a connotation that suggests that ketamine is much too powerful for human consumption. At high doses, ketamine’s dissociative state leads to hallucinations of a visual or auditory type.
Ketamine had been used in psychiatric work as early as the 1970s in Mexico, Argentina, Iran, and Soviet Union. The protocols utilized time-limited treatments rather than long-term dosing, and just like other psychedelics, ketamine was utilized with other psychotherapeutic approaches.
More recently, ketamine is found efficacy in the treatment of depression and PTSD. It is only recently that mental health providers have found use for ketamine to any regular degree. Initially, in the 1990s, Yale researchers used ketamine to study symptoms of schizophrenia, as ketamine mimics schizophrenia symptoms. These symptoms are known as psychomimetic effects. Ultimately, it was found that ketamine was effective in depression treatment. Ketamine works on the glutamate system as opposed to traditional antidepressants. Ketamine stimulates brain-derived neurotrophic factor (BDNF) formation, which is frequently described as “fertilizer for the brain.” BDNF increases the growth of new brain cells, synapse formation, and new connections between brain cells.
What is ketamine-assisted therapy (KAP)?
There is a pharmaceutical framework for the use of ketamine, where ketamine is administered alone without any integration or psychotherapy. There is also ketamine-assisted psychotherapy (KAP), where psychotherapy is included as part of the treatment.
With the mechanical administration of ketamine, there is no talk therapy or minimal talk therapy, and the effects last 7 to 14 days, which requires repeat dosing. The experience of the ketamine treatment is not discussed, and interpersonal issues are not focused upon. KAP represents a methodology where low to moderate doses of ketamine are delivered so that an altered level of consciousness occurs that facilitates psychotherapy. The framework for this can include low to high ketamine doses with KAP occurring during a therapeutic setting or talk therapy that occurs during and following the experience with integration sessions. There can be preparatory sessions as well.
Higher doses of ketamine produce major shifts in perceptions with mystical type experiences and feelings of ego dissolution. For some, they will undergo ego death. These can be negative feelings if the person is not prepared and supported during and afterwards. In KAP therapy, an individual may undergo psychotherapy immediately after the effects of ketamine dissipate and also within the days to weeks that followed, in which the experience and emotions are examined. The goal is to stabilize positive behavioral changes, resolve psychological issues, improve relationships, enhance self-awareness, catalyze new insights, and consolidate psychological material.
Ketamine Therapy: A Disruptive Treatment Paradigm

Ketamine can be used as a lubricant in the psychotherapy process. It is important that the patient participate in the right treatment, and as such, it is important not to attribute all the benefits of ketamine to just the biochemical properties, but rather consider that maybe the psychomimetic side effect has a role in the healing process. The psychomimetic side effect is not something that needs to be avoided or medicated away, as it may be a way to increase psychological flexibility and resolve psychological issues. Ketamine can be used in the context of an ongoing psychotherapy relationship and administered in a number of different ways: through intravenous routes, oral lozenge, and through intramuscular injections (0.3-.8 mg/kg). The goal of the integration sessions with the therapist is to have consolidation of psychological material, but the treatment session is not the time to go searching for new memories, but rather resolve difficult issues without intellectualizing them. The patient “knows” the concepts after the integration.
Working in higher doses during the therapeutic setting, we can get mystical and psychedelic experiences. These can certainly provoke anxiety without adequate preparation. The dose is typically 1 to 2 mg per kilogram intramuscular, after which patients have vid dream-like visions that last up to 50 minutes. Patients can feel as if they are “dissolved” as they enter a dissociative and transpersonal space. Many will describe “divine energy”, “sense of oneness or completeness”, and “a sense of cohesion with the world.” These mystical visions are valued in the treatment process. The integration process involves the assistance of helping the patient to construct meaning from their visions and identify actions they should take to have wellness. It is unknown which treatment regimen will ultimately work for which patient.
What makes ketamine different is not that it only affects the glutamate system but also that it is legal to use. Ketamine offers the opportunity to have a psychedelic, transpersonal and dissociative experiences. Ketamine leads to expanded mental states and mood modulation.
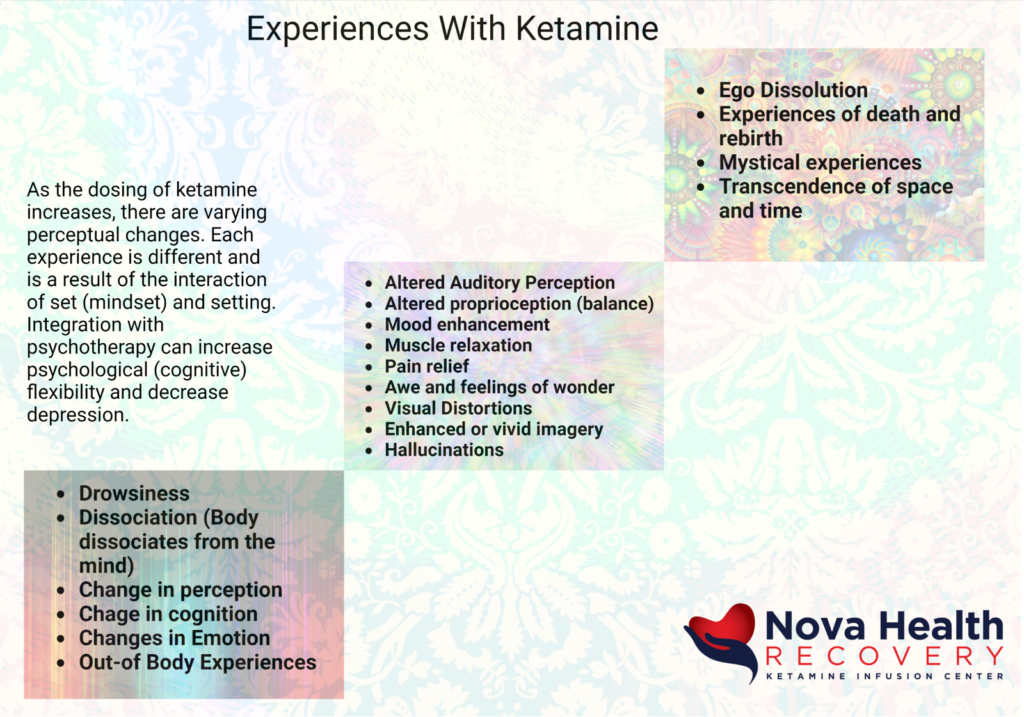
The experiences of ketamine:
The ketamine experience varies based on the route of administration, the dose, the mindset of the patient, and the setting. Each experience will be different and requires integration psychotherapy to maintain maximum effect. It is well-known that cognitive behavioral therapy has efficacy in its antidepressant effect, and studies demonstrate that adding CBT to ketamine therapies may prolong the antidepressant effect of ketamine treatments. The benefit of preparation psychotherapy sessions may allow the person to bring focus attention for the upcoming journey and prepare for any unconscious mental states that this individual was not aware of. It allows you to address expectations, concerns, and hopes of the process, as well as reflect on your understanding of the mystical experience in cosmic consciousness states that you may achieve during the ketamine infusion. Certainly, an individual can have an intention for the treatment process, but they should not be upset if the particular journey that they expected does not occur. It is important to integrate both beneficial and negative experiences during the ketamine infusion so that the person can learn from each session.
General experiences become more enhanced as the dosing gets higher with ketamine. Initially there may be a sense of numbness and heaviness with difficulty speaking. For many there will be drowsiness, enhanced visuals, vivid imagery, and changes in perception or cognition. Some will become very emotional in both positive and negative ways. There are also auditory perceptual changes, with music causing movement internally in the individual’s journey. As the dosing gets higher, there can be dissociation of the body from the mind, out-of-body experiences, visual hallucinations, transcendence of space and time, mystical experiences, and experiences of death and rebirth.
Many of these experiences are not able to be properly described by the individual (ineffability), but it is important for them to Journal these experiences in broad terms, whether it is with drawings, writing, cutting out pictures from magazines that may be similar to their experiences, or other methods.
Psychotherapeutic applications for ketamine use:
Ketamine has been used in several different disorders, but the following conditions have been effectively treated with ketamine:
- OCD
- Treatment resistant depression
- Suicidality
- Pain with depression
- Posttraumatic stress disorder
- Substance use disorders
- Anxiety
- Anorexia
- Chronic relational problems
- Severe treatment resistant depression
- Ruminative suicidal ideation
- Bipolar depression
Examples of KAP studies demonstrating efficacy of the combination of ketamine and psychotherapy are listed below. Each of these studies utilized ketamine in the context of psychotherapeutic modalities.
Azhari N., Hu H., O’Malley K. Y., Blocker M. E., Levin F. R., Dakwar E. (2021). Ketamine-facilitated behavioral treatment for cannabis use disorder: a proof of concept study. Am. J. Drug Alcohol. Abuse 47, 92–97. doi: 10.1080/00952990.2020.1808982, PMID: [PubMed] [CrossRef]
An uncontrolled trial of eight people with cannabis use disorder, 1-2 ketamine infusions over four weeks with infusion number one at .71 mg per kilogram over 52 minutes on week two for non-responders 1.41 mg per kilogram over 92 minutes on week four and six weeks of motivational enhancement therapy and mindfulness-based relapse prevention occurring outside the ketamine administrations. Motivational enhancement therapy (MET) therapy the day before the infusion and the afternoon of the infusion.
Wilkinson S. T., Rhee T. G., Joormann J., Webler R., Ortiz Lopez M., Kitay B., et al.. (2021). Cognitive behavioral therapy to sustain the antidepressant effects of ketamine in treatment-resistant depression: A randomized clinical trial. Psychother. Psychosom. 90, 318–327. doi: 10.1159/000517074, PMID: [PubMed] [CrossRef]
41 patients randomized controlled trial with severe major depressive disorder- six IV infusions Ketamine (o.5 mg/kg over 40 minutes) over three weeks with 14-week program of cognitive behavioral therapy versus 14 patient’s treatment as usual. CBT was administered outside of ketamine administration.
Wilkinson S. T., Wright D., Fasula M. K., Fenton L., Griepp M., Ostroff R. B., et al.. (2017). Cognitive behavior therapy may sustain antidepressant effects of intravenous ketamine in treatment-resistant depression. Psychother. Psychosom. 86, 162–167. doi: 10.1159/000457960, PMID: [PMC free article] [PubMed] [CrossRef]
16 patients in uncontrolled trial with major depressive disorder given for infusions of ketamine at 0.5 mg per kilogram over 40 minutes over two weeks in 10-week program of cognitive behavioral therapy given outside of ketamine infusions.
Shiroma P. R., Thuras P., Wels J., Erbes C., Kehle-Forbes S., Polusny M. (2020). A proof-of-concept study of subanesthetic intravenous ketamine combined with prolonged exposure therapy among veterans with posttraumatic stress disorder. J. Clin. Psychiatry 81, 20l13406. doi: 10.4088/JCP.20l13406, PMID: [PubMed] [CrossRef]
12 patients in a non-controlled trial with chronic post-traumatic stress disorder given three IV infusions of ketamine at 0.5 mg/kg over 40 minutes once weekly for the first three weeks. Then treatment with 10 weeks of progressive exposure with therapy during ketamine administrations.
Sappington A. A., Corssen G., Becker A. T., Tavakoli M. (1979). Ketamine-facilitated induced anxiety therapy and its effect upon clients’ reactions to stressful situations. J. Clin. Psychol. 35, 425–429. doi: 10.1002/1097-4679(197904)35:2<425::aid-jclp2270350240>3.0.co;2-9, PMID: [PubMed] [CrossRef] [Google Scholar]
21 patients in a randomized controlled trial, all healthy given .1 mg per pound IV ketamine infusion to induce anxiety. This is “induced- anxiety” therapy focused on induction of negative affect prior to drug administrations. Drug-induced relaxation and processing with therapist present.
Rodriguez C. I., Wheaton M., Zwerling J., Steinman S. A., Sonnenfeld D., Galfalvy H., et al.. (2016). Can exposure-based CBT extend IV ketamine’s effects in obsessive-compulsive disorder? An open-label trial. J. Clin. Psychiatry 77, 408–409. doi: 10.4088/JCP.15l10138, PMID: [PMC free article] [PubMed]
10 patients at uncontrolled trial with obsessive-compulsive disorder given a single IV ketamine infusion 0.5 mg per kilogram over 40 minutes with 10 sessions of exposure response prevention therapy over two weeks. Therapy occurred outside of ketamine administration.
Pradhan B., Mitrev L., Moaddell R., Wainer I. W. (2018). d-Serine is a potential biomarker for clinical response in treatment of post-traumatic stress disorder using (R,S)-ketamine infusion and TIMBER psychotherapy: a pilot study. Biochim. Biophys. Acta, Proteins Proteomics 1866, 831–839. doi: 10.1016/j.bbapap.2018.03.006 [PMC free article] [PubMed] [CrossRef]
20 patients in a randomized controlled trial of refractory posttraumatic stress disorder given single IV infusions ketamine at 0.5 mg per kilogram over 40 minutes with 12 sessions of timber-(trauma interventions using mindfulness-based extinction and reconsolidation)
Krupitsky E. M., Burakov A. M., Dunaevsky I. V., Romanova T. N., Slavina T. Y., Grinenko A. Y. (2007). Single versus repeated sessions of ketamine-assisted psychotherapy for people with heroin dependence. J. Psychoactive Drugs 39, 13–19. doi: 10.1080/02791072.2007.10399860, PMID: [PubMed] [CrossRef] [Google Scholar]
59 patients in a randomized controlled trial with heroin use disorder with the treatment group given three intramuscular ketamine injections at 2 mg per kilogram with one month intervals between doses whereas the control group got a single intramuscular ketamine injection at 2 mg per kilogram with addiction counseling and ketamine psychotherapy administered before during and after ketamine administration.
Krupitsky E., Burakov A., Romanova T., Dunaevsky I., Strassman R., Grinenko A. (2002). Ketamine psychotherapy for heroin addiction: immediate effects and two-year follow-up. J. Subst. Abus. Treat. 23, 273–283. doi: 10.1016/s0740-5472(02)00275-1, PMID: [PubMed] [CrossRef] [Google Scholar]
70 patients in a randomized controlled trial of heroin use disorder with the treatment group given single intramuscular ketamine at 2 mg per kilogram in the control group given .2 mg per kilogram using ketamine psychotherapy methods before during and after ketamine.
Krupitsky E. M., Grinenko A. Y. (1997). Ketamine psychedelic therapy (KPT): a review of the results of ten years of research. J. Psychoactive Drugs 29, 165–183. doi: 10.1080/02791072.1997.10400185, PMID: [PubMed] [CrossRef] [Google Scholar]
111 non-randomized controlled trial of alcohol use disorder patients getting ketamine 2.5 mg per kilogram IM in two non-traditional medications and using ketamine psychotherapy before during and after ketamine therapy.
Khorramzadeh E., Lotfy A. O. (1973). The use of ketamine in psychiatry. Psychosomatics 14, 344–346. doi: 10.1016/S0033-3182(73)71306-2 [PubMed] [CrossRef] [Google Scholar]
One-hundred patients in a non-randomized controlled trial receiving IV ketamine infusions at three dose ranges of .2 to .3 mg per kilogram, .4-.6 mg per kilogram, .7-1.0 milligram per kilogram with abreactive psychotherapy during drug administration. Unknown duration.
Grabski M., McAndrew A., Lawn W., Marsh B., Raymen L., Stevens T., et al.. (2022). Adjunctive ketamine with relapse prevention-based psychological therapy in the treatment of alcohol use disorder. Am. J. Psychiatry 179, 152–162. doi: 10.1176/appi.ajp.2021.21030277, PMID: [PubMed] [CrossRef] [Google Scholar]
96 patients in a randomized controlled trial of alcohol use disorder receiving three weekly IV ketamine infusions at 0.8 mg per kilogram IV over 40 minutes and seven sessions of mindfulness-based relapse prevention in the treatment group. Mindfulness-based relapse prevention and alcohol education was provided before and 24 hours after infusion.
Dore J., Turnipseed B., Dwyer S., Turnipseed A., Andries J., Ascani G., et al.. (2019). Ketamine assisted psychotherapy (KAP): patient demographics, clinical data and outcomes in three large practices administering ketamine with psychotherapy. J. Psychoactive Drugs 51, 189–198. doi: 10.1080/02791072.2019.1587556, PMID: [PubMed] [CrossRef] [Google Scholar]
235 patients in observational study with mixed problems given, sublingual and intramuscular ketamine at doses between 200 to 250 mg sublingual and 80 to 90 mg intramuscular. Outpatient ketamine assisted psychotherapy were two weeks apart or more frequently the number of sessions between one and 25 spread over variable times.
Dakwar E., Levin F., Hart C. L., Basaraba C., Choi J., Pavlicova M., et al.. (2020). A single ketamine infusion combined with motivational enhancement therapy for alcohol use disorder: a randomized midazolam-controlled pilot trial. Am. J. Psychiatry 177, 125–133. doi: 10.1176/appi.ajp.2019.19070684, PMID: [PubMed] [CrossRef] [Google Scholar]
40 patients in a randomized controlled trial of alkyl use disorder given a single IV ketamine infusion at .71 mg per kilogram over 52 minutes whereas control groups were given IV midazolam. There was five-week outpatient motivational enhancement therapy with six sessions of MET over five weeks which occurred outside of ketamine administration. MET was provided after the infusion.
Dakwar E., Nunes E. V., Hart C. L., Foltin R. W., Mathew S. J., Carpenter K. M., et al.. (2019). A single ketamine infusion combined With mindfulness-based behavioral modification to treat cocaine dependence: A randomized clinical trial. Am. J. Psychiatry 176, 923–930. doi: 10.1176/appi.ajp.2019.18101123, PMID: [PubMed] [CrossRef]
55 patients in a randomized controlled trial of cocaine use disorder with the treatment group given a single ID ketamine fusion 0.5 mg per kilogram over 40 minutes in a five-week inpatient-outpatient program of mindfulness-based relapse prevention. There were eight sessions of mindfulness-based relapse prevention twice weekly for four weeks.
Psychological Flexibility to Improve Psychotherapy
Psychological flexibility is lost in treatment-resistant depression. Psychological flexibility is an individual’s ability to recognize and adapt to contextual demands, maintain balance in life domains, be aware of and committed to behaviors consistent with values, and shift mindset or behaviors during individual and social experiences. (1) Ways to measure psychological flexibility include the acceptance and action questionnaire (AAQ-II), and psychological flexibility in its measurement mediates the relationship between acute psychedelic effects and subsequent decreases in depression and anxiety. (2) (3) Acceptance and commitment therapy (ACT) can be effective for treatment-resistant depression. (7) ACT emphasizes psychological flexibility, and this may be a useful tool in psychedelic-assisted treatments such as ketamine therapy.(8) (9) ACT may increase the adaptability of an individual’s behaviors and their mindset such that they are able to balance new behaviors and step away from old, less effective behaviors.
The set and setting of the environment in which the psychedelic drug is administered influences the therapeutic value of the psychedelic effects. (4)(5) In other words, the context in which the psychedelic is given influences therapeutic outcomes based on a number of research studies. (6)(5)
Ketamine therapy will require integrations of varying types. Ketamine therapy will most likely have a longer impact on patients when psychotherapy is co-prescribed. The type of psychotherapy that is ultimately found to be best has yet to be determined. Traditional models like cognitive behavioral therapy and acceptance and commitment therapy are just examples of therapies that are of value in the psychedelic realm. Whether during a ketamine infusion, the therapy is “experience oriented” or “plasticity oriented” , therapies must focus on outcomes of improving psychological flexibility in lowering cognitive rigidity that is common in patients with treatment-resistant depression. It is not uncommon for a patient to get “stuck” in therapy, with hamster wheel thought processes that are endless and obsessive in tone. Ketamine therapy and other psychedelic may offer the ability to have psychotherapy work better, but whether this therapy is administered during the psychedelic experience or after the psychedelic experience is variable in practice, in the best treatment paradigm has yet to be rigidly evaluated. An integrative approach to ketamine therapy with multiple layers of psychotherapy will be critical to achieving long-term success in mood disorders. (11) The same can be said with addiction disorders, in which there is also a lack of psychological flexibility that results in compulsive use. Evidence suggests that ketamine and psychotherapies may be of value in breaking the cycle when combined with appropriate therapy.
(1) Kashdan T. B. (2010). Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 30, 865–878. doi: 10.1016/j.cpr.2010.03.001, PMID: [PMC free article] [PubMed]
(2) Close J. B., Hajien E. C., Watts R., Roseman L., Carhart-Harris R. L. (2020). Psychedelics and psychological flexibility – results of a prospective web-survey using the acceptance and action questionnaire II. J. Contextual Behav. Sci. 16, 37–44. doi: 10.1016/j.jcbs.2020.01.005 [CrossRef]
(3) Davis A. K., Barrett F. S., Griffiths R. R. (2020). Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. J. Contextual Behav. Sci. 15, 39–45. doi: 10.1016/j.jcbs.2019.11.004, PMID: [PMC free article] [PubMed]
(4) Hartogsohn I. (2016). Set and setting, psychedelics and the placebo response: An extra-pharmacological perspective on psychopharmacology. J. Psychopharmacol. 30, 1259–1267. doi: 10.1177/0269881116677852, PMID: [PubMed]
(5) Carhart-Harris R. L., Roseman L., Haijen E., Erritzoe D., Watts R., Branchi I., et al.. (2018). Psychedelics and the essential importance of context. J. Psychopharmacol. 32, 725–731. doi: 10.1177/0269881118754710, PMID: [PubMed] [CrossRef]
(6) Garcia-Romeu A., Richards W. A. (2018). Current perspectives on psychedelic therapy: use of serotonergic hallucinogens in clinical interventions. Int. Rev. Psychiatry 30, 291–316. doi: 10.1080/09540261.2018.1486289, PMID: [PubMed]
(7) Bai Z., Luo S., Zhang L., Wu S., Chi I. (2020). Acceptance and commitment therapy (ACT) to reduce depression: a systematic review and meta-analysis. J. Affect. Disord. 260, 728–737. doi: 10.1016/j.jad.2019.09.040, PMID: [PubMed] [CrossRef]
(8) Wolff M., Evens R., Mertens L. J., Koslowski M., Betzler F., Gründer G., et al.. (2020). Learning to let go: a cognitive-behavioral model of how psychedelic therapy promotes acceptance. Front. Psychol. 11:5. doi: 10.3389/fpsyt.2020.00005, PMID: [PMC free article] [PubMed]
(9) Sloshower J., Guss J., Krause R., Wallace R. M., Williams M. T., Reed S., et al.. (2020). Psilocybin-assisted therapy of major depressive disorder using acceptance and commitment therapy as a therapeutic frame. J. Contextual Behav. Sci. 15, 12–19. doi: 10.1016/j.jcbs.2019.11.002 [CrossRef]
(10) Walsh Z., Thiessen M. S. (2018). Psychedelics and the new behaviourism: considering the integration of third-wave behaviour therapies with psychedelic-assisted therapy. Int. Rev. Psychiatry 30, 343–349. doi: 10.1080/09540261.2018.1474088, PMID: [PubMed] [CrossRef]
(11) Muscat S.-A., Hartelius G., Crouch C. R., Morin K. W. (2021a). An integrative approach to ketamine therapy may enhance multiple dimensions of efficacy: improving therapeutic outcomes with treatment-resistant depression. Front. Psychol. 12:710338. doi: 10.3389/fpsyt.2021.710338, PMID: [PMC free article] [PubMed]
(12) Walsh Z., Mollaahmetoglu O. M., Rootman J., Golsof S., Keeler J., Marsh B., et al.. (2021). Ketamine for the treatment of mental health and substance use disorders: comprehensive systematic review. BJPsych Open 8:e19. doi: 10.1192/bjo.2021.1061, PMID: [PMC free article] [PubMed]
Read the dropdown menus below regarding the Four Stages of KAP Therapy:
KAP Therapy – The experience and How It Works
Ketamine Assisted Psychotherapy – the experience and how it works
Ketamine has a long track history of safety in the anesthetic arena, for which it was approved in 1970. Ketamine has been used in the outpatient setting and more recently for psychiatric use as well. An extensive body of literature experience supports this safety for both office use and for use by patients at home alone. (1) The potential of ketamine to treat psychological and psychiatric problems has been evaluated since the early 1970s. The first use in mental health disorders was by Khorramzadeh and Lofty in 1973 (2) and then in Argentina as an antidepressant psychotherapy by Fontana et al. (3). Other practitioners also utilized ketamine therapy for other conditions such as addiction with the work of Krupitsky and Grinenko. (4) Since these times, there have been numerous other evaluations of the use of ketamine as it integrates with psychotherapy.
So, ketamine has been used since the early 1970s as a method of self-exploration and psychotherapeutic contexts even before the study by Berman et al. in 2000 in which ketamine was used intravenously on treatment-resistant depression patients with robust and rapid results. It was recognized that traditional antidepressant treatments with SSRIs and SNRIs did not work rapidly or effectively, and other treatments were in need. The evaluation of the antidepressant value of ketamine was looked at starting in 1994 by Krystal et al. in which they were looking into the psycho mimetic and perceptual changes that occurred with ketamine use and later applied it to patients who are depressed.
The treatment paradigm for depression was initially 0.5 mg/kg IV ketamine over 40 minutes, which resulted in a rapid and robust decrease in depression that only lasted a short while.In fact, it was noted that there could be remission of treatment-resistant depression and reduced suicidality.(6) So, the key is to lengthen the efficacy and duration of ketamine’s effect. The other issue with the medical studies of ketamine is that the dissociative effects were considered to be unwanted; however, there appears to be benefit from psychedelic experiences which parallel findings seen in psilocybin studies, in which mystical experiences improve treatment outcomes. (7) (8) It appears that the psychedelic effects may improve mental health and well-being. The psychedelic effects of ketamine have been vilified by individuals who are biased that somehow this is a bad thing. In fact, the psychedelic effects are part of the therapeutic flow of these treatments and improving mood disorders.
Ketamine therapies are extremely safe. Ketamine is used in anesthesia and is noted to have fewer cardiovascular effects than other medications. Ketamine has been on the World Health Organization’s essential medication list since 1985 because of its safety and efficacy as an anesthetic agent. Repeat dose ketamine has also been found to be extremely safe in the treatment of mood disorders.(9) It has been found that ketamine can be used not just in the operating room but also in outpatient settings for pain management as well as mental health. Sublingual ketamine and oral ketamine can be used at lower doses to create a trance-like state, in which the individual can interact with their therapist during a KAP session, or ketamine can be used at higher intramuscular doses to create a deeper journey that requires subsequent integrations.
Ketamine was discovered by Calvin Stevens in 1962, and FDA approved in 1970. Multiple routes of ketamine administration can be used, including intravenous, intramuscular, intranasal, sublingual, and oral delivery. Each of these methods has its advantages, and some make office and home use more convenient.
Ketamine works as an NMDA receptor antagonist and affects the glutamate system of the cortex. The glutamate system is an excitatory system that is involved with learning and pain. Glutamate dysregulation can cause loss of neuroplasticity and depression. When ketamine is administered, it produces a brief glutamate burst that allows the production of neuroplastic proteins such as brain derived neurotrophic factor (BDNF) which then allows for protein production involved in new synapse production. This allows for neural plasticity and new neural connections which improve cognitive functioning and mood. Ketamine also impacts other neurotransmitter systems such as the opioid system, the GABA system, monoamine systems, and cholinergic systems.
When ketamine is administered for depression, many patients will note dizziness, derealization, and drowsiness. These are considered to be adverse effects by many; However, these may be of therapeutic benefit and represent part of the treatment process.(10) The safety and tolerability of ketamine has been noted in numerous studies. (11) There have been no persistent neuropsychiatric problems, medical effects or increase in substance abuse in clinical practice with the use of ketamine.
Ketamine assisted psychotherapy – The experience
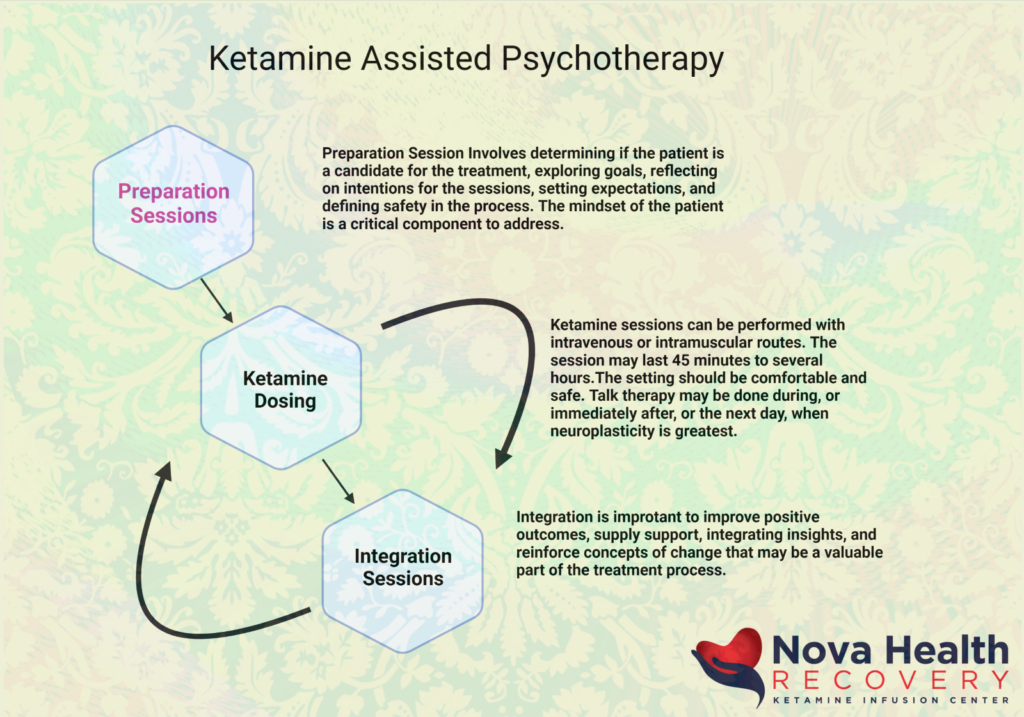
There are a number of formats by which Ketamine assisted psychotherapies (KAP) are administered. There is always a preparation session, in which the individual is assessed to see if they are appropriate for ketamine therapy. The patient’s goals are explored, intentions are evaluated and reflected upon, expectations are assessed, and safety is defined in the process. The individual is given information regarding the safety of the setting. It is important that the mindset of the individual be appropriately framed. This can impact the experience of the ketamine infusion.
The next step is the ketamine dosing, in which either intravenous, sublingual, or intramuscular routes are used. The sessions may last anywhere from 45 minutes to several hours. It is important that the setting be comfortable, warm, inviting, and homelike to create an atmosphere that the individual feels comfortable and safe in. Talk therapy to be done during the ketamine infusion or can be done immediately after the infusion.
Integration sessions are important to improve positive outcomes, integrate insights, reinforce concepts of change, and supply support through the treatment process.
The experience of the ketamine infusion is almost like a timeout from ordinary states of consciousness. Mind expansion, in which the person’s thoughts are allowed to roam, allows an individual to access themselves in a larger manner. The individuals may be more vulnerable and open with their expansiveness of mind, and this enhances psychotherapy during and after the administration of ketamine. The integration serves as a process to help the individual recover from their depression and trauma and integrated in a way that is more meaningful for them to learn from.
Lower dose KAP sessions can be used with sublingual ketamine or low dose IV and IM ketamine to promote increased communication between therapist and client and allow the individual to face difficult states of mind with less fear. Individuals may find relief from their depression and obsessions. The individuals will need to activate their inner healer and get a sense of the newness they have come upon. KAP sessions are generally multiple sessions scattered over several weeks to months.
Higher dose KAP Sessions (IM 30-140 mg) can produce an out of body experience, with ego dissolution and reduction of body and sensory awareness. There are changes in visual, auditory, and tactile sensations. Sensory perceptions are distorted, and there can be hallucinations or visions. Individuals at these higher doses will have difficulty verbalizing or intellectualizing their experiences.
In both lower and higher dose ketamine assisted psychotherapy sessions, a number of different effects can be noted. The individual will have sensory changes such as increased connectedness and appreciation for formerly irrelevant things. They will have increased connectivity and unique experiences during the infusion. Their mind will float and roam freely while observing themselves from a different direction. Most individuals will not be able to direct the experience, hence the issue with setting intentions can be problematic in that the actual ketamine experience is not necessarily going to proceed the way it was intended. Individuals may also experience formlessness and a cosmic consciousness that is greater than themselves. This is close to a state of ego-dissolution.
Many times, especially in higher dose ketamine infusions or treatments, time gets distorted – it lengthens or shortens. The individual may float and not feel attached, and yet they may feel connected – which seems contradictory. Some may have apprehension of death during the experience. Some will note that they are stretching or shrinking. This may give many a perspective of humility and that there is a larger view of the universe than just themselves, but they may still feel that there is greater purpose and meaning in their lives. Some patients will move during the infusion, scream, or shake. Although shaking and screaming is alarming to the guide and staff, it is best not to interrupt the flow as this can be an important part of their therapy.
Integration
Psychological flexibility is one of the key areas that needs improvement in mood disorders. It is important after the ketamine treatment that fixed thinking and circular thinking are addressed. The new sense of self needs to be reviewed in terms of how the individual will move forward from this point. Individuals may sense increased creativity, resilience, and hope. These thoughts should be journaled as well as reviewed by the therapist. Many individuals will have reductions in their negative sense of self and more trust in their mental stability. Individuals will need to learn to structure their new lifestyles to become more effective, and learn to put away the depressed mentality and behaviors that had been destructive to them before. Integration sessions are critical in establishing these goals.
KAP Therapy Results
The number of KAP sessions to treat a particular condition is unknown, however, multiple sessions are generally required for treatment results. KAP therapy significantly decreases depression and anxiety, especially in individuals with higher Beck Depression Inventory scores, suicidality, psychiatric hospitalizations, and pediatric trauma. (12)
Conditions treated by KAP
ketamine assisted psychotherapy has been utilized in a number of different mood disorders which include:
- treatment resistant depression
- obsessive-compulsive disorder
- posttraumatic stress disorder
- addiction disorders
- relationship problems
- personality disorders
- anxiety disorders
- existential crises
- bipolar depression
- Generalized anxiety disorder
- Other
Conclusions:
Ketamine therapy offers a rapid treatment for mood disorders that have formally had minimal success with traditional therapies. Ketamine works through a different neurotransmitter system than other available agents. The main issue with ketamine therapies is that it is short acting and requires repeat dosing. Efforts to increase the response rate and the length of response have had little success, but the addition of psychotherapy sessions in a sequenced manner before, during, and after ketamine treatments has demonstrated improvement in the number of domains. Ketamine therapy cannot be used in isolation and solely as a medical treatment. The psychedelic effects of ketamine represent part of the treatment response that is important to be kept as opposed to being medicated away. The psychedelic effects allow individuals to have greater responses to ketamine as well as to psychotherapy. It is important to incorporate integration therapies in order to consolidate the new positive direction that many individuals take as a result of the treatments.
- Collins, K., J. Murrough, A. Perez, D. Reich, D. Charney, and S. Mathew. 2010. Safety and efficacy of repeated-dose intravenous ketamine for treatment-resistant depression. Biological Psychiatry 67 (2):139–45. Crossref. PubMed.
- Khorramzadeh, E., and A. Lofty. 1973. The use of ketamine in psychiatry. Psychosomatics 14:344–46. Crossref. PubMed.
- Fontana, A. 1974. Terapia atidepresiva con ketamine. Acta psiquiatrica y psicologica de America latina 20:32. PubMed.
- Krupitsky, E., and A. Grinenko. 1997. Ketamine psychedelic therapy (KPT)—A review of the results of ten years of research. Journal of Psychoactive Drugs 29 (2):165–83. Crossref. PubMed.
- Krystal, J. H., L. P. Karper, J. P. Seibyl, G. K. Freeman, R. Delaney, J. D. Bremner, and D. S. Charney. 1994. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans: Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Archives of General Psychiatry 51 (3):199–214. Crossref. PubMed.
- Krystal, J. H. 2007. Ketamine and the potential role for rapid-acting antidepressant medications. Swiss Medical Weekly 137 (15–16):215–16. PubMed.
- Luckenbaugh, D. A., M. J. Niciu, D. F. Ionescu, N. M. Nolan, E. M. Richards, N. E. Brutsche, and C. Zarate. 2014. Do the dissociative side effects of ketamine mediate antidepressant effects. Journal of Affective Disorders 159:56–61. Crossref. PubMed.
- Griffiths, R., M. Johnson, W. Richards, B. Richards, U. McCann, and R. Jesse. 2011. Psilocybin occasioned mystical-type experiences: Immediate and persisting dose-related effects. Psychopharmacology (Berl) 218 (4):649–65. Crossref. PubMed.
- Collins, K., J. Murrough, A. Perez, D. Reich, D. Charney, and S. Mathew. 2010. Safety and efficacy of repeated-dose intravenous ketamine for treatment-resistant depression. Biological Psychiatry 67 (2):139–45. Crossref. PubMed.
- McGirr, A., M. Berlim, D. Bond, M. Fleck, L. Yatham, and R. W. Lam. 2014. A systematic review and meta-analysis of randomized, double-blind, placebo-controlled trials of ketamine in the rapid treatment of major depressive episodes. Psychological Medicine. Crossref. PubMed.
- Jaitly, V. 2013. Sublingual ketamine in chronic pain: Service evaluation by examining more than 200 patient years of data. Journal of Observational Pain Medicine 1/2 (2013).
- Dore J, Turnipseed B, Dwyer S, Turnipseed A, Andries J, Ascani G, Monnette C, Huidekoper A, Strauss N, Wolfson P. Ketamine Assisted Psychotherapy (KAP): Patient Demographics, Clinical Data and Outcomes in Three Large Practices Administering Ketamine with Psychotherapy. J Psychoactive Drugs. 2019 Apr-Jun;51(2):189-198. doi: 10.1080/02791072.2019.1587556. Epub 2019 Mar 27. PMID: 30917760.
Preparation Sessions for KAP Therapy
Preparation Sessions for Ketamine Assisted Psychotherapy (KAP)
There are several aspects in ketamine therapies for the treatment of mood disorders that should be considered:
- The medical aspect: Ketamine therapy can be considered a medical procedure alone, and this is the case in many ketamine treatment centers. There certainly are some medical interventions that would be utilized in any ketamine session, such as the use of medication for nausea or monitoring heart rate or blood pressure. Solely placing the ketamine infusion as the only source of healing would be incorrect, as psychotherapy is necessary to integrate any new learning and prolong the effects and duration of ketamine treatment. The medical aspect looks primarily at the neurobiological mechanisms in which paradigm, ketamine works in isolation from any psychological input.
- The psychological and psychotherapeutic aspects include increasing psychological flexibility in learning new adaptive responses with the improvement of mood using psychotherapy. This is the integration portion of treatment that allows individuals to address new concepts they may have developed during the treatment process. Ketamine therapy lubricates the psychotherapeutic process to promote symptom reduction and benefit medical treatment with ketamine. Psychotherapy supports the patient throughout the process of this treatment.
- The psychedelic/transpersonal aspect of treatment includes the deeper transformational state in which healing can occur that is outside of just what is achieved with psychological treatment alone.
There are also several methods with which ketamine treatment is provided in conjunction with psychotherapy, and these include:
- Ketamine treatment in the medical setting with psychotherapy followed up at some later time
- Preparation sessions with the therapist, therapy during the ketamine session, and then integration sessions
- Ketamine sessions with the presence of a therapist as a guide and monitor
- Ketamine-assisted psychotherapy, in which the therapist engages the patient during the ketamine treatment session, at which time the patient is more able to communicate freely as their defense mechanisms may be less engaged.
Certainly, important aspects of this are the set and setting as well as an interpersonal connection. The set is the mindset of the patient with their prior expectations and intentions brought into the session. The set could also include more recent adverse interactions that may be on the mind of the individual. The setting refers to the actual location and place in which the treatment occurs, which generally should be safe and comfortable, warm and inviting. There is also the need for interpersonal connection between the patient and their therapist. The therapist that understands and knows the patient and is trusted by the patient can connect better during the ketamine session than anybody else. So, there is the therapeutic relationship as a primary container in which the physician and the medication support create, and psychotherapy with preparation and integration that is built into this treatment plan. Altered states of consciousness become a crucial part of the healing process in the treatment of mood disorders as they are ways to decrease cognitive rigidity.
Below are some of the rooms at NOVA Health Recovery Ketamine Treatment Center in Alexandria, Virginia, that reflect a calm, minimally medicalized, and safe setting for KAP therapy. Therapists are invited to perform treatment sessions during or after a ketamine session.

The setting of a ketamine treatment room at NOVA Health Recovery Center with as minimal medicalization as possible and space for the therapist to be present.

The setting of a ketamine treatment room at NOVA Health Recovery Center.

The setting of a ketamine treatment room at NOVA Health Recovery Center
So, we have the following for an effective ketamine assisted psychotherapy session:
- Preparation
- Set and setting
- The therapeutic relationship between the patient, therapist, and physician
- The ketamine session
- Integration sessions, at which time insights and concepts can be reinforced when positive, and negative features can be addressed as well in order to improve positive outcomes
.
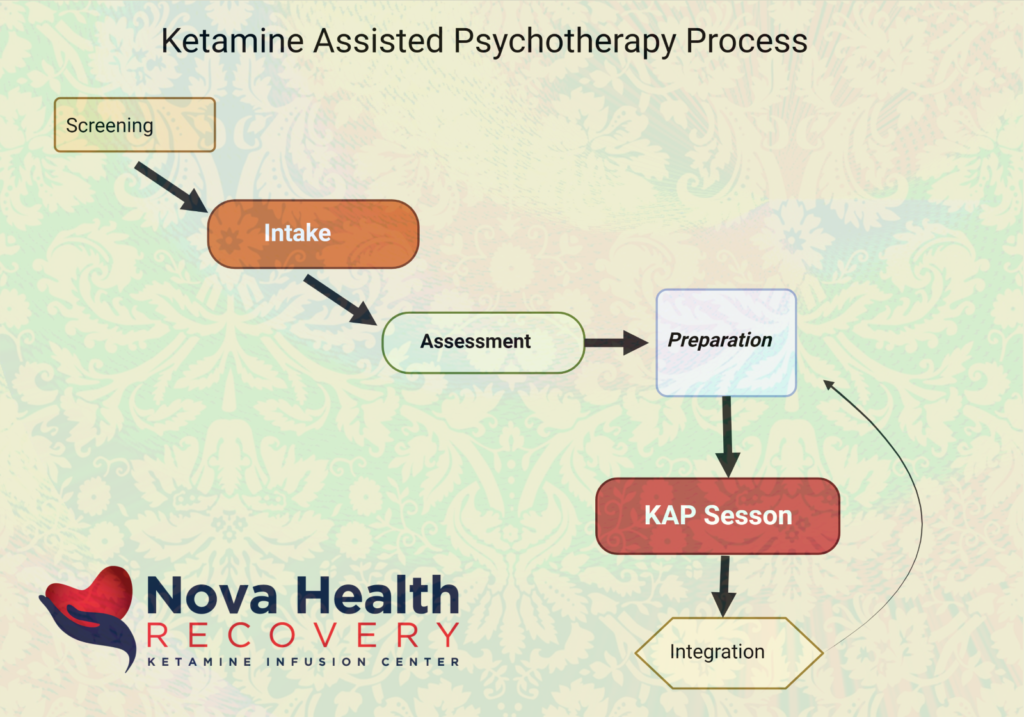
The ketamine process begins with the following:
- Screening: A patient or physician/Therapist reaches out to see if ketamine is a good choice for the mood disorder. Patients can self-refer, and therapists can refer patients to NOVA Health Recovery. Certain key issues may reveal that the person is not a great candidate for this treatment, such as medical conditions. These negative conditions include recent heart attack, recent stroke, lung-related issues, kidney failure, liver failure, non-ambulatory status, pregnancy, or schizophrenia. Certain personality disorders may also not be improved with ketamine therapies. Diagnoses that are benefited by ketamine therapies with psychotherapy would include: treatment-resistant depression, postpartum depression, bipolar depression, anxiety, OCD, PTSD, and certain existential crises.
- Intake: When the patient comes to the office, a mental health and medical evaluation can be established which allows the involved staff to learn the mental health journey of the patient as well as any physical dilemmas that have arisen, including addiction disorders and medical complications. What has the patient lost during that journey?
- Assessment: Assessment is part of the intake process, and this can include medical assessment for medical complications as well as possible mental health complications that ketamine may not address. Issues such as uncontrolled blood pressure, uncontrolled diabetes, and other health-related concerns can be addressed at this stage. Many patients are non-compliant due to their mental health crisis and loss of cognitive abilities. For patients with addiction disorders, medical concerns such as hepatitis C, HIV, and other medical concerns may need to be evaluated.
- Preparation: The goals of preparation are to obtain informed consent, establishing a safe container for the patient so that they recognize that this treatment is not to be feared, and that it will be performed in a safe and comfortable environment. Treatment expectations need to be set with the patient as well, and the patient needs to understand that this is a non-linear treatment process. This means that sometimes the patient will feel better, sometimes a treatment may do nothing for them, and occasionally they may feel worse after a treatment. The length of the treatment process can vary as well from patient to patient. It is important to create optimal treatment conditions and plan for integration after ketamine sessions. Items that are included in this whole process of preparation are establishing the set and setting, in which the rooms are adjusted comfortably, and provisions are made for a sense of safety and comfort. Music is also an important preparation, as it can guide the flow of the individual’s journey. Ambient music is best, especially when it is unrecognized, because some music may have negative consequences for some clients. Sometimes, when the patient recognizes a song, it may take them out of their journey. It is also important to prepare the patient regarding their expectations and possible experiences, and that they may have varying thoughts throughout the entire process, kind of like a lazy river of thoughts. Certainly, a support system of therapists, friends, and family may be of value in the process. Regulation techniques in preparation of their body are also important parts of the preparation process. Explaining to the patient the importance of breathing and grounding themselves during the infusion may allow them to travel through difficult experiences during the infusion. Likewise, fasting and resting prior to the treatment are important so that the individual is more relaxed upon initiation of treatment.
- Informed consent: it is important that during the preparation process, the expectations of the treatment are readdressed in that there are specific agreements around the setting in the role of touch. If the patient dissociates and seems to be in distress, it is best to address whether or not they want medication to calm them down or merely a touch to the shoulder to remind them that they are in a safe place. Some individuals do not want to be touched at all, and once these parameters are set, they should not be crossed during the infusion when the patient is altered. It is also important to have a discussion of aftercare when the patient is done with their treatment. Any medications that will be utilized in the process of the caving session should also be addressed, especially ones for nausea and dizziness.
- The set of ketamine-assisted psychotherapy plays a key role in the experience of the client. This refers to the mindset of the client and the therapist as well as cultural and societal norms that may impact the person’s journey. The client must be able to understand that they will be having altered states of consciousness. They need to be aware that there is not an absolute manner with which to prepare for the experience, but recognize that a difficult experience can be life-changing in positive ways as can fantastic experiences of altered states of consciousness. The goals of overall treatment should be addressed as well as an intention for each session. The client must understand that the intention might not be ultimately what is achieved during a session, but not to be upset with that or feel that they have failed because their intention during the session was not met.
- Other principles for these treatments include discussions with the client that they need to trust and activate their inner healing intelligence. The healing comes from within and all ketamine treatments, and the purpose of having the therapist along with the medication is to help guide the patient in a more positive direction. The ketamine session is also an experiential learning experience in which healing can occur through the direct experience of altered states of consciousness. Patients must direct their inner healing self towards positive outcomes.
- Somatic preparation: Experiences are stored in the body. It is important to recognize that childhood adverse consequences, as measured in the Aces score, are linked to increased mental illness, increased inflammation, increased substance use problems, chronic health problems, and impact fulfillment in life. Trauma from events earlier in life, as well as recently, can be frozen in the body, so it is important not to leave out somatic therapies and bodywork from the healing and psychedelic part of the process. It is important to recognize that individuals may shake or move during the ketamine sessions as a way of relieving somatic experiences within the body. This may be distressing to the provider but may be a form of release to the patient. Other aspects of somatic preparation include areas such as nourishment ( diet, supplements, water), exercise and physical strength, balance (Yoga), sleep and rejuvenation, rest and replenishment (massage/acupuncture), and somatic therapies which allow processing, releasing and reintegrating new information.
- Music: one last revisiting of music as part of the set. It is important to be flexible around the patient’s preferences but ambient music with changing styles and textures are more beneficial than ones with lyrics which can be distracting and confusing. It is better to use unfamiliar music as it brings surprise and decreases predictability. Also, familiar music may trigger the patient, especially if the music is associated with a prior negative memory.
- As the session is about to start, consider the setting one last time with a reminder of the rules of the treatment process, such as no standing up and expectations surrounding therapeutic touch. Also review the intention setting one last time as well as a shift into the space of medicine. Music, aroma, and grounding materials such as furniture placement and other local items should be noted so that the patient feels safe and comfortable.
The Ketamine Session:
Now that the preparation session is completed, the ketamine experience can begin. There are varying ketamine experiences which include:
- Low-dose psycholytic therapy which leads to empathogenic states and trance-like moods but allows for verbal communication (best for active KAP)
- Moderate dose treatments thatcan be out-of-body experiences or floating sensations.
- Moderate to high dose sessions which create near-death experiences
- higher dose ketamine treatments thatlead to ego dissolution and transformational experiences ( K Hole)
During these treatments, an individual can have varying altered states of consciousness in which they may experience multiple journeys such as a perinatal realm of consciousness, as if they were in the uterus again, or they may experience a mythological realm of consciousness, or even a mystical realm of consciousness. Individuals can sometimes look inward or step out of their bodies to look at themselves, or they can connect with nature and the more archetypal realm of consciousness. Each treatment will be different, and each experience will be different. Some treatments will be exciting and mood lifting, but some may be challenging journeys. These offer opportunities for reframing fixed beliefs that have become a part of the depression experience. The benefit of these altered states of consciousness is new experiential learning that can be translated to more positive mood outcomes and cognitive flexibility.
Integration:
The integration sessions are immensely important in consolidating gains after the ketamine session. Integration can be initiated immediately after the ketamine session or the following day or days. The sessions are designed to supply support and reinforce concepts of change. They also can address difficult situations that may have arisen during the ketamine session.
The Ketamine Session in KAP

Ketamine Assisted Psychotherapy – The ketamine session
The ketamine session consists of several components, including the medical construct, which involves the neurobiological mechanisms by which ketamine works as well as the actual medical administration of ketamine. There is also a psychological component that involves changes in psychological flexibility, changes in mood, In the reinforcement of positive insights as well as reprocessing negative components. The transpersonal component represents the actual psychedelic journey that the individual undergoes and experiences. Ultimately what is left behind is the signature of ketamine treatment, which is the neuro-biochemical effects that ketamine therapy produces after its administration. This involves neuroplasticity that increases cognitive flexibility and allows individuals to process issues and process the transpersonal state and the phenomenon associated with it. The goal of all of this is symptom reduction, and psychotherapy is involved in expediting that process along with any material that comes out during states of altered consciousness.
It is important to understand that depression has its roots not just in genetics, but also other processes such as inflammation, hormonal disorders, chronic stress, trauma of multiple types ( developmental, interpersonal, single incident, military), environmental issues (mold, heavy metals, environmental pollutants), lifestyle issues, addictions, personality disorders, poverty, economic distress, racial trauma, political trauma, and pain. These sources of depression will need to be addressed during the integration process as they may become more present during the ketamine sessions.
Ketamine therapy is rapid in onset and undergoes a rapid metabolism, such that the improvements seen in mood last way longer than the actual ketamine is present in the system. Ketamine has an excellent safety profile and is used in sub anesthetic dosing for the treatment of mood disorders. The one issue with this type of treatment is that booster infusions or treatments are required, and it has been demonstrated that adding psychotherapy during the process allows for increased durability and improvement of mood disorders.
The ketamine experience involves a reduction or elimination of external stimuli with heightened internal visuals as well as an increased connection to the symbolic realm of experiences. This treatment reduces negative and obsessive thoughts, especially self-referential thinking that is typically seen in depression due to the default mode network being highly over-activated. Ketamine also allows for mind expansion with a sense of spaciousness of the mind and a sense of movement. Depression is more or less a closed down and dark sensation that ketamine improves through the phenomenon of mind expansion. In other words, the cognitive rigidity that is seen in depressed states is replaced with cognitive flexibility. In order for an individual to comfortably go into an altered consciousness, they must recognize they will experience a loss of control or surrender and that at higher doses of ketamine therapy, they will have multiple sensations that can be contradictory such as formlessness, interconnectedness, a sense of humility, religiosity, and spirituality. They may undergo archetypal experiences and encounters, and even out-of-body experiences. Some may even have ego death. These experiences are dose-related during the ketamine treatments, and variations of ketamine infusion during an actual session can be such that the initial part of the treatment can allow verbal communication between the patient and therapist, but later in the session, the dosing can be increased to give the dissociated state. Whether the experience is uplifting and amazing, or whether it is a challenging experience, either will allow for change and growth to occur.
During the ketamine session, the set and setting are critical in allowing the person to maximize their experience and personal growth. Frequently, music is an essential part of the journey. Music allows for an internal experience, as well as an internal focus, if the patient prefers not to converse during the session. In that case, the therapist is there to provide support should it be needed. It is also critical for the patient to feel comfortable and safe. the primary container is the physician and medication, which supports psychotherapy. The preparation before the ketamine session and the integration, thereafter, are part of the entire treatment plan.
Preparation—> Set and Setting —> Therapeutic Relationship —> Integration
Some final words about the set and setting include that the patient should check in with the providers and the provider should check in with the patient to see if there are any concerns, set intentions, obtain feedback on prior sessions that should be changed for this session, and set ground rules. The lighting and music should be adjusted for maximal comfort. Also, discussing what worked and what didn’t work with the patient also allows for the process to be fine-tuned. There can certainly be a shift to a more ceremonial space during the initiation of the ketamine session. Some individuals will find the experience to be more life-changing and that there should be more ceremony involved during the process for some. The use of a tuning fork, a ringing bell, or an invocation such as a poem can be used to start the process of the ketamine experience as it transitions from the medical realm to the transpersonal realm. Keep in mind that it is important that during the ketamine session, the provider does not intrude on the process when the patient seems to be distressed in an emotional fashion. Individuals under the ketamine experience may be processing trauma in a new way and any intrusion may interfere with this process. It is important to remain available when these distressed states arise and provide comfort and safety so that the patient can process the experience. Certainly, after the infusion is done, individuals can slowly talk and reflect on the experience until they are ready to leave.
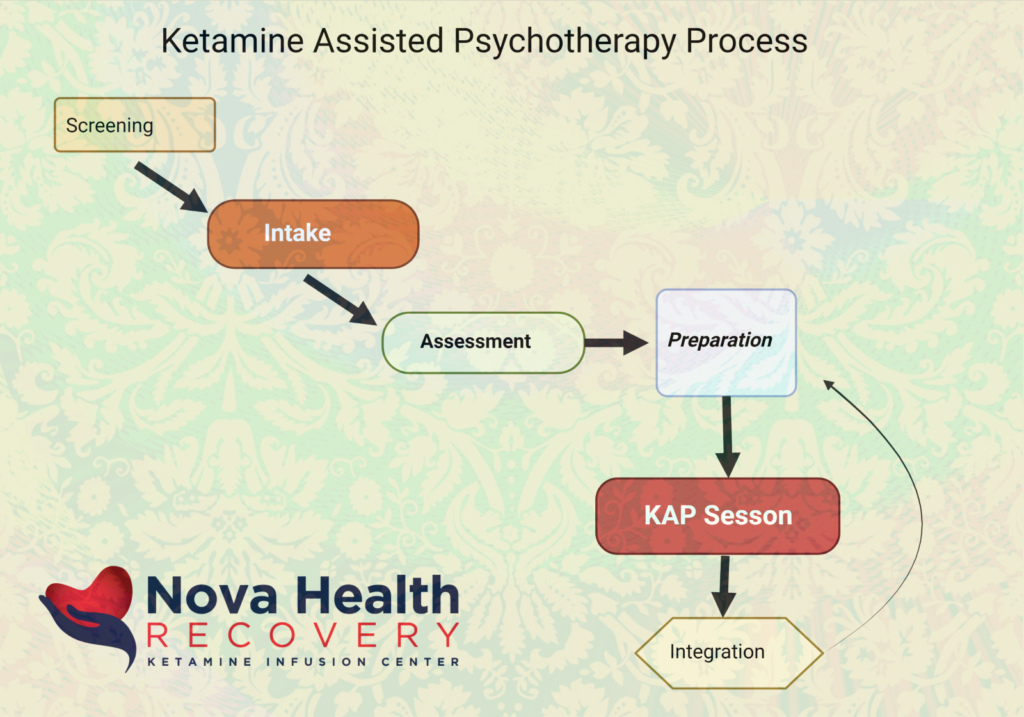
There are multiple treatment protocols using KAP therapy and depression. For intravenous ketamine therapies, generally, there are 2 to 3 sessions per week for 2 to 4 weeks. In KAP sessions, or maybe two sessions per week for up to 3 to 4 weeks. Further initial sessions may be required for some patients, but generally, booster sessions may vary from weekly to every 2 to 3 weeks with a gradual extension between booster sessions as patients improve. Some patients will do well with at-home treatments using intranasal or oral ketamine. Group sessions may also be utilized as a form of the treatment process, and home-based nasal spray ketamine or oral ketamine is used for the experience.
There are certain principles for ketamine-assisted psychotherapy that are important to understand. These include:
- The patient must have trust and activation of their inner healing intelligence. Ultimately it is up to them to alter their lifestyle, incorporate a new sense of their selves, and become behaviorally activated in order to maintain the effectiveness of the treatment.
- Ketamine-assisted psychotherapy is an inner-directed approach. Again, the healing starts from within.
- KAP involves experiential learning, in which healing occurs through direct experience. This experience comes in the form of altered states of consciousness.
The ketamine experience can be varied depending on the dosing administered. So, there are several types of ketamine experience:
- Lower dose psycholytic therapy which allows the individual to be verbally responsive but places them in a trance-like state.
- Moderate dosing treatments in which the person may have out-of-body experiences
- Moderate to high dose ketamine treatments produce near death-like experiences.
- High dose ketamine can produce transformational experiences otherwise known as “ego death”
The treatment process with KAP does require some contingencies. Occasionally, some patients get more emotional and even express suicidal ideation. This may be in part due to increased sympathetic arousal that occurs from ketamine treatments. It is often common to have an increase in sympathetic arousal, which results in insomnia, anger, rage, and fight or flight symptoms. This can lead to increased emotionality and anxiety. Some patients may voice suicidal thoughts because they feel they have not improved. Assessment of this, as well as protocols to deal with the situation, should be in place. Other considerations are made for those that do not respond to this treatment, for many of the patients will tell the clinician that this is their last chance for any treatment to work. Finally, many patients to improve through this therapy will have lost significant time, money, family, and jobs through their mental health journey. Now they will have to process all that loss in a meaningful way. This is an important part of integration – the processing of losses due to past depression. The issue of improved mental health also takes a twist in that some individuals will suddenly have the energy to make life-changing decisions such as quitting a job or leading a relationship. It is best for individuals to give a little bit of time after the treatments before they go about making such large decisions.
Among the many goals of KAP therapy, new habits and coping skills are critical. The slow return to an emotionally regulated state may take multiple sessions. For some individuals, it is difficult for them to return to traditional therapy when they are unable to process emotions without the assistance of an altered state of consciousness. What is required in these cases is the use of home-based ketamine therapies to augment psychotherapy. NOVA Health Recovery Ketamine Treatment Center offers home-based ketamine therapy with oral and intranasal ketamine administered in a prescriptive manner. This can be utilized as a lubricant for more effective psychotherapy in the office setting.
Therapists have the opportunity to provide therapy sessions during and immediately after ketamine sessions at the office. Integration sessions can be timed for optimal responses to ketamine infusions. The administration of ketamine therapies and monitoring is done through the staff at NOVA Health Recovery. Home-based ketamine prescriptions are also prescribed through a medical prescription that enables patient use for assisting in psychotherapy sessions at a therapist’s office.
The Integration Session in KAP
Ketamine-assisted psychotherapy Integration
Integration sessions follow the ketamine dosing sessions. The goal is to promote positive outcomes by supplying support, integrating insights, and reinforcing concepts of change as well as assessing things that did not change during the treatment process. Effectively, integration is a process of releasing old information, processing the experience in new information, reclaiming your old self, re-inhabiting older constructs you left behind because of depression, and restoring your life to a more effective state.
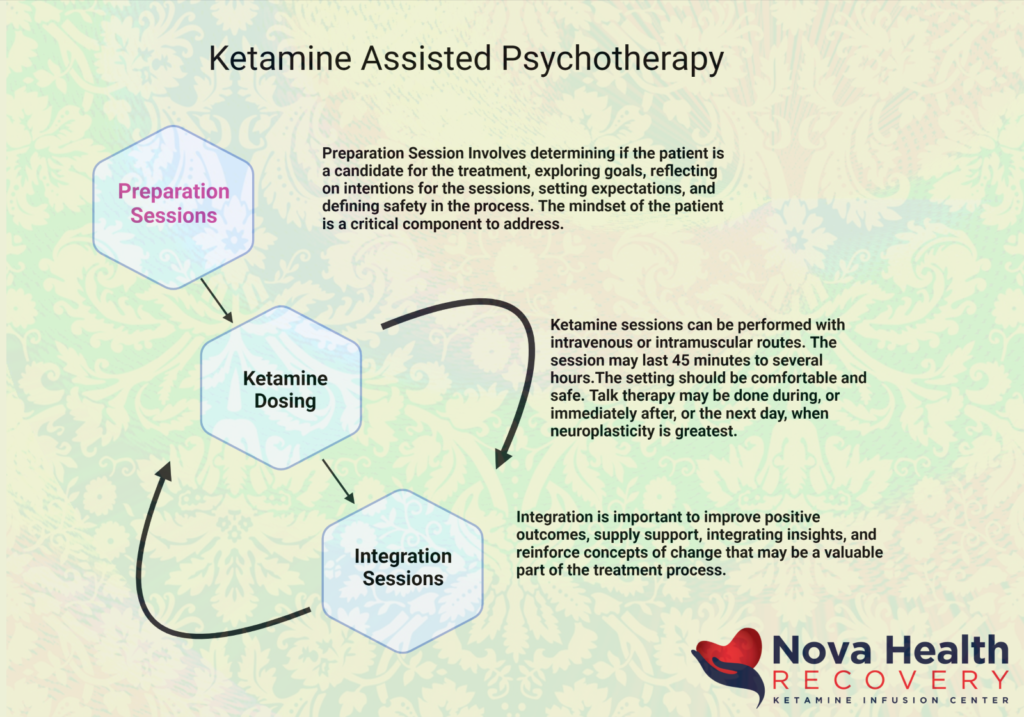
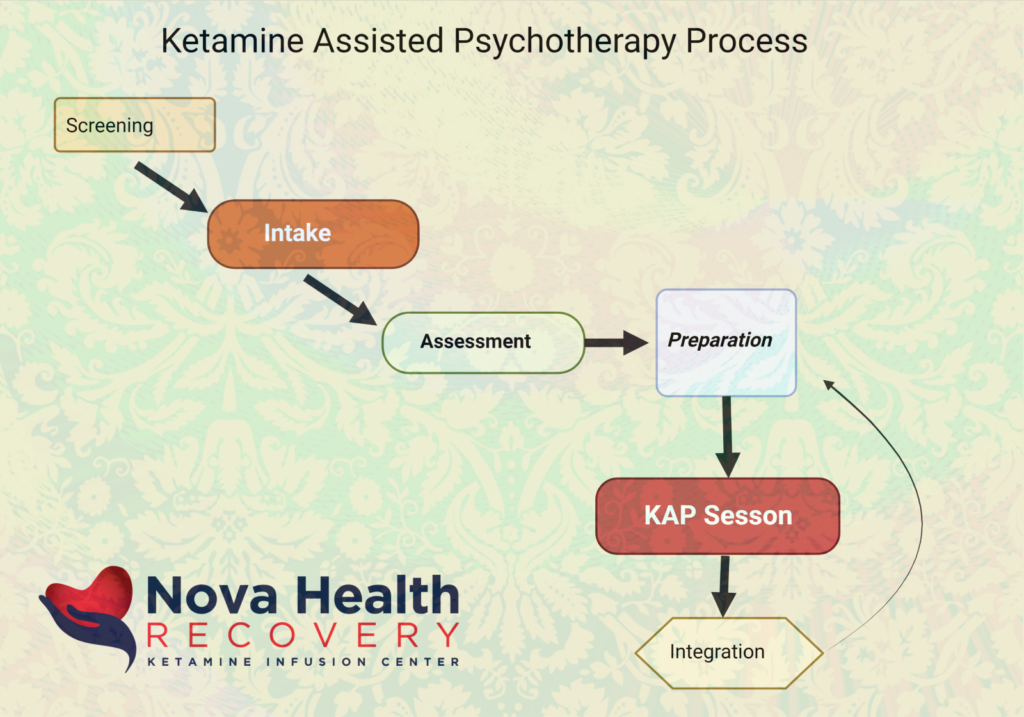
Integration occurs at a number of different levels including the personal level (ego or biographical level), the somatic level, and the transpersonal level with symbolic, spiritual, transgenerational effects as well.
The goal of integration includes the following:
- Supplying support to a rapidly changing individual. This also includes debriefing from difficult or challenging experiences during the ketamine sessions.
- Integrating new insights and reinforcing concepts of change
- Application of newfound insights and promoting their longevity.
- Emotional processing with release and grieving.
- Enhanced self-monitoring and observing the ego.
- Adapting to new changes in your identity, worldview, and relationships. Learning to embrace these changes and trust them.
- Establishing the meaning of these newfound concepts.
- Somatic integration is also important because experiences are stored in the body, especially childhood adverse experiences. Trauma can be frozen into the body, and it is important to not leave the body out of therapy healing during psychedelic work. Somatic integrations include appropriate nourishment, rest/sleep, embodiment (movement and dance), alignment ( chiropractic work), exercise, and detoxification (fasting, sweating).
- Trauma integration is also critical. Ketamine therapies allow for choice, something that individuals with trauma did not have. It may be difficult for individuals with trauma to trust the experience. The purpose of trauma integration includes transforming pathological shame into dignity, restoring natural responses in the nervous system, empowerment, and connection with a more benign spirituality.
During the ketamine session, it is important to allow for verbalization and recollection of the person’s journeys and to debrief them and allow them to process this information whether it was an enjoyable and enhanced experience or a challenging experience. It is also important to allow the person to return into the body and provide support by emphasizing movement, smell, and anchoring. This is called embodiment support. It is also important to ensure safety before the person leaves with appropriate stabilization, especially if the person has had suicidal ideation.
The challenges of integration in KAP Therapy
There are a number of challenges that occur in integration. These include the following:
- Nonlinear improvements: sometimes patients will have amazing KAP sessions, and then other ones will not go so well, and the client will question whether they got the correct ketamine dosing when in fact, it was just part of the process of nonlinear improvement that we see with KAP therapy. Some sessions may produce neutral or negative ‘results’ while others are very productive.
- Compliance: many individuals will not follow up after the initial sessions only to relapse back into depression.
- Relationship impacts: Sometimes, the client will improve so much that their significant other loses their identity as a caretaker now that the client is feeling so much better. This can put stress on the relationship when the partner is overbearing or doting and no longer feels they play a role as a caretaker.
- Negative therapeutic reaction: Sometimes, individuals would get specific feelings or delusions under the medication and have difficulty deciding if it is real or if it was from Ketamine.
- Rapid changes in lifestyle: some individuals feel so good that they make life-changing decisions such as changing jobs or getting divorced.
For integration to work it must provide beyond the goal of just symptom relief. It is important for the individual to:
- Engage with their inner healer and not just take a passive role in their mental health journey
- Individuals must adapt to their newfound symptom relief and not identify themselves as generally symptomatic.
- Focusing on the individual’s life and not the medicine or the journey is important.
- Have an increased sense of well-being
- Increase clarity and self-regulation.
- Connecting with one’s feelings and allowing increased emotionality but maintaining regulation
- Increased socialization with friends and family
- Bring back change a little bit at a time so as to not be overwhelmed. Sometimes, it is important to focus on what has changed as opposed to focusing on what has not changed and to bring back a structured lifestyle a bit at a time.
Integration sessions can start immediately after the dosing session and can be repeated multiple times as each condition necessitates. There are no hard rules as to how many sessions one would need, but more frequent sessions seem to improve results and duration. Integration sessions can take place the following few days after the ketamine session.




Ketamine Facts

NOVA Health Recovery Ketamine Infusion Center
NOVA Health Recovery Ketamine Infusion Center Has been treating patients with Treatment-resistant depression, PTSD, Anxiety disorders, and bipolar depression for over 7 years, with over 12,000 infusions performed as well as hundreds of KAP sessions. We utilize home-based oral and intranasal ketamine therapies for maintenance treatments as well as to help lubricate traditional psychotherapy for office-based therapists.


